 February 2016
February 2016
Radiology Billing and Coding: Medicare Fee Schedule — Mostly Positive for Radiologists In 2016
By Lonnie Johnson, MBA, and Missy Lovell, BSN, RN, MBA
Radiology Today
Vol. 17 No. 2 P. 32
The final rule for the Medicare Physician Fee Schedule (MPFS) was released on October 30, 2015, and radiologists can anticipate more positive and fewer negative changes and impacts. The Centers for Medicare & Medicaid Services (CMS) estimates the overall impact of the MPFS changes to diagnostic radiology to be 0% while IR will see an aggregate increase of 1%, and nuclear medicine a decrease of 1%. Following are highlights of the key provisions of the final rule.
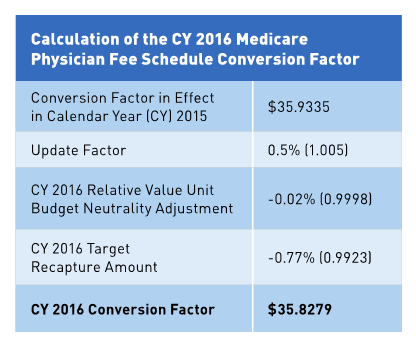
Slightly Lower Conversion Factor
The conversion factor (CF) for 2016 is $35.8279, which is slightly less than the 2015 CF of $35.9335. Many expected to see it increase overall, but the 2016 CF reflects various adjustments, including a budget neutrality adjustment; the +0.5% update adjustment factor specified under the Medicare Access and CHIP Reauthorization Act (MACRA); the 0.77% target recapture amount, required due to misvalued code reduction target provisions contained in the Protecting Access to Medicare Act (PAMA); and the Achieving a Better Life Experience Act of 2014. The calendar year (CY) 2016 Target Recapture Amount will include a reduction to the CF of -0.77% s illustrated in the accompanying table.
Potential Raise in Practice Expense May Impact BVU
CMS, according to the ACR, is readying their proposal to update the cost of a PACS workstation to $5,557 from the current price of $2,501, explaining that the latter price was based on the proxy item and the former based on submitted invoices. They add that this should positively impact the practice expense relative value units (RVU) for affected services.
Clinical Decision Support Delayed
In this MPFS final rule, CMS does not intend to require that ordering professionals meet the appropriate use criteria/clinical decision support (CDS) requirement by January 1, 2017.
In the PAMA, Congress required that providers who order advanced diagnostic imaging services consult with appropriate use criteria via a CDS mechanism. CMS is "required to specify appropriate use criteria from among those developed or endorsed by national medical professional specialty societies and other provider-led entities," according to the ACR. Additional components required by the PAMA include the following: CMS approval of CDS mechanisms, collection of additional data on the Medicare claim form, and the development of a prior authorization program based upon the claims data.
In late 2015, CMS announced the implementation of the first component of this program in this MPFS final rule with a comment period by establishing which organizations will be eligible to develop or endorse appropriate use criteria. CMS states that it anticipates including further discussion and adopting policies regarding claims-based reporting requirements in the CY 2017 and 2018 rulemaking cycles.
Lung Cancer Screening: Hurry Up and Wait
Since the publication of the final rule, billing instructions have been released by CMS. Although the ACR recommended that the LDCT (G0297) RVU crosswalk to 71250 (CT, thorax; without contrast material) with additional physician work added to account for the added intensity of the service, CMS disagreed with the additional work component. CMS also maintained that the physician work (time and intensity) is identical in both G0297 and 71250, and finalized identical work RVU for 2016.
Changes for CT Under the PAMA 2014
Section 218(a)(1) of the PAMA mandates that for the technical component of applicable CT services paid under the MPFS and the 2014 Hospital Outpatient Prospective Payment System that a 5% reduction in 2016, and a 15% reduction in 2017 and subsequent years be made for services furnished using equipment that does not meet the requirements of the National Electrical Manufacturers Association (NEMA) Standard XR-29-2013.
To implement this provision, CMS will create modifier CT services furnished using equipment that does not meet each of the attributes of the NEMA XR-29-2013 standard.
CMS has since stated that beginning on January 1, 2016, claims for CT scans with specified CPT codes (and any successor codes) that are furnished on non-NEMA Standard XR-29-2013-compliant CT scans must include modifier CT, and said modifier will result in the applicable payment reduction for the technical component service.
PQRS … Up to 2018
CMS reiterates that the Physician Quality Reporting System (PQRS) encourages individual eligible professionals (EPs) and group practices to report information on the quality of care and that the 2018 PQRS payment adjustment is the last adjustment that will be issued under the PQRS program.
Starting in 2019, according to CMS, adjustments to payment for quality reporting and other criteria will be made under the Merit-Based Incentive Payment System (MIPS), as required by MACRA. CMS sought comment related to other MACRA provisions in the CY 2016 PFS proposed rule, as well as in a previously published request for information.
CMS finalized requirements for the 2018 PQRS payment adjustment consistent with the requirements for the 2017 PQRS payment adjustment, and made changes to the PQRS measure set to add measures where gaps exist, as well as to eliminate measures that are topped out, duplicative, or are being replaced. CMS has added a potentially relevant measure for many radiology professionals that can be submitted via claims and through a qualified registry: Measure #436: Radiation Consideration for Adult CT: Utilization of Dose Lowering Techniques.
Transition to MIPS
The value-based modifier (VBM) "provides for differential payments under the MPFS to physicians, groups of physicians, and other EPs based on the quality and cost of care they furnish to beneficiaries enrolled in the traditional Medicare fee-for-service program," according to CMS.
The final VBM policies are intended "to help provide a smooth transition" from the current program to MIPS as it, like PQRS, is set to expire at the end of CY 2018. The 2018 payment adjustments are the last adjustment that will be issued under the current quality programs. Starting in 2019, adjustments to payment for quality reporting and other factors will be made under the MIPS, as required by MACRA.
CMS uses 2016 as the performance period for the 2018 Value Modifier and will continue to apply the CY 2018 Value Modifier based on participation in the PQRS by groups and solo practitioners.
While these changes are not so new that radiologists will be taken aback, there are still some impacts and policy updates that radiologists should consider now, while anticipating more changes outlined through 2018.
— Lonnie Johnson, MBA, is vice president of corporate services with Zotec Partners.
— Missy Lovell, BSN, RN, MBA, is compliance manager with Zotec Partners.
Resources
1. ACR preliminary summary of radiology provisions in the 2016 MPFS final rule. American College of Radiology website. http://www.acr.org/News-Publications/News/News-Articles/2015/Economics/20151030-ACR-Preliminary-Summary-of-Radiology-Provisions-in-the-2016-MPFS-Final-Rule. Updated October 30, 2015.
2. Proposed policy, payment, and quality provisions changes to the Medicare Physician Fee Schedule for Calendar Year 2016. Centers for Medicare & Medicaid Services website. https://www.cms.gov/Newsroom/MediaReleaseDatabase/Fact-sheets/2015-Fact-sheets-items/2015-10-30-2.html. Updated October 30, 2015.

