By Ashok Madan, MD, PhD; Rathnakar Sherigar, MD;
and Lisa Bates, RDMS
History
A 60-year-old man presented to the emergency department with acute onset right testicular pain and swelling after doing some heavy lifting during the last couple of days. The patient reported pain radiating to the lower abdomen. He denied dysuria, urethral discharge, or any fever or night sweats and also said he had not been sexually active for the past six years.
The patient’s past medical history included cirrhosis, hepatitis C, benign prostate hypertrophy, hypertension, type 2 diabetes, and remote repair of right inguinal hernia.
A clinical exam revealed the visibly uncomfortable seated patient had a right scrotum that was tender, swollen, and warm to the touch, with no discreet palpable right inguinal hernia.
Findings
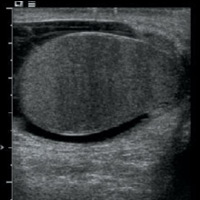
An ultrasound examination showed heterogeneously hypoechoic, mildly enlarged, diffusely hypervascular right epididymis and testes with impressively increased color and pulsed Doppler flow (Figures A, B, and C). There appeared to be multiseptated complex fluid in the right scrotum encasing the right testes and epididymis, most appreciably in the cephalad right scrotum, depicting complex reactive hydrocele/pyocele (Figure F). There also was a 1.5-cm multiloculated complex collection within the right epididymal head reflecting a small abscess (Figures D and E).
Diagnosis
Acute right epididymo-orchitis with reactive complex hydrocele/pyocele and epididymal head abscess
Discussion
Epididymo-orchitis is inflammation of the epididymis and testes. Most cases are caused by sexually transmitted diseases or retrograde ascent of pathogens from the urinary tract. Approximately 20% to 40% of cases of epididymitis are associated with orchitis, mostly due to direct extension of the infection into the testicular parenchyma. Bimodal distribution with peak incidence occurs in men aged 16 to 30 and a second peak occurs between the ages of 51 and 70.
Clinical presentation may be acute, subacute, or chronic. Acute presentation characterized with abrupt onset often involves unilateral scrotal pain and swelling, often with referred pain to the lower abdomen. Urinary tract infection symptoms such as dysuria, hematuria, fever, and flank pain may occur concomitantly. Pain relief with testicular elevation (Prehn’s sign) may be elicited, although it is unreliable. Cremasteric reflex remains intact.
Risk factors include sexual activity, strenuous physical activity, bicycle or motorcycle riding, and long travel while seated. People with a sedentary lifestyle, including diagnostic radiologists, also are at risk.
Common etiologies include sexually transmitted diseases such as Neisseria gonorrhoeae and chlamydia in the younger patient population and Escherichia coli with anal intercourse. Other pathogens include Klebsiella, Pseudomonas, Proteus and, in rare cases, Mycobacterium. HIV and immune-suppressed patients have an additional risk of developing a fungal or viral infection, including Cytomegalovirus. Blood-borne dissemination is rare and more often associated with isolated orchitis.
Noninfectious causes may be related to congenital anatomic anomalies (posterior urethral valves, meatal stenosis) or benign prostate hypertrophy in older men.
Treatment entails empiric treatment based on the most likely pathogen prior to completing laboratory testing. Symptomatic relief can be found with analgesics, limitation of physical activity, scrotal elevation, and the use of hot and cold packs.
— Ashok Madan, MD, PhD, is a staff radiologist at the Salem VA Medical Center in Virginia.
— Rathnakar Sherigar, MD, is chief of radiology at the Salem VA Medical Center.
— Lisa Bates, RDMS, is a sonographer at the Salem VA Medical Center.
 |
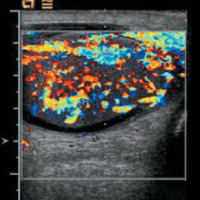 |
| Figure A | Figure B |
 |
 |
| Figure C | Figure D |
 |
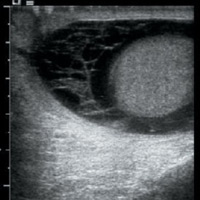 |
| Figure E | Figure F |
- Trojian TH, Lishnak TS, Heiman D. Epididymitis and orchitis: an overview. Am Fam Physician. 2009;79(7):583-587.
- Kaver I, Matzkin H, Braf ZF. Epididymo-orchitis: a retrospective study of 121 patients. J Fam Pract. 1990;30(5):548-552.
- Kim W, Rosen MA, Langer JE, Banner MP, Siegelman ES, Ramchandani P. US-MR imaging correlation in pathologic conditions of the scrotum. Radiographics. 2007;27(5):1239-1253.
Submission Instructions
- Cases should have clinical relevance and clear radiological findings.
- Seconds should include a title, history and course of illness, findings, diagnosis, and discussion.
- Word count should not exceed 800. At least three references are recommended.
- Cases may be submitted from any radiological subspecialty and imaging modality.
- Figures must be high-quality JPEG or TIFF images and labeled for ease of reference. Please keep images in their native format, without the addition of arrows or other means of highlighting the key findings.
Submit cases via e-mail to Rahul V. Pawar, MD, at rvp325@gmail.com or to Radiology Today at jknaub@gvpub.com.
Department of Radiology, Division of Neuroradiology
Saint Barnabas Medical Center/Barnabas Ambulatory Care Center