By Heather J. Wichman, MD, and Venkataramu N. Krishnamurthy, MBBS
History
A 75-year-old man with a complicated medical history, including atrial fibrillation, congestive heart failure, and chronic pancreatitis, presented to our emergency department with the chief complaint of shortness of breath and dizziness. Initial laboratory findings were significant for a low hemoglobin level (7.5 mg/dL).
Review of his outside medical records indicated that three months prior to his visit to our institution, he had a hemoglobin level of 6.4 mg/dL and a left hemothorax. The hemothorax was felt to have been caused by spontaneous bleeding due to supratherapeutic anticoagulation from warfarin therapy for atrial fibrillation.
Findings
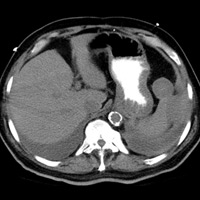
During admission in our facility, noncontrast abdomen/pelvis CT was performed due to the history of supratherapeutic anticoagulation and anemia. The CT scan revealed a perisplenic hematoma and a round low-density lesion contiguous with the upper pole of the spleen (Figure A).
An ultrasound was subsequently performed to determine cystic or solid characteristics of the splenic lesion. Color Doppler imaging revealed a 4.6 X 3.9 cm anechoic lesion with two jets of arterial flow within the lesion, corresponding to the low-density CT lesion (Figure B).
Diagnosis
Intraparenchymal pseudoaneurysm
Treatment
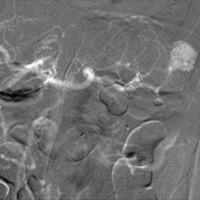
The patient was taken to the interventional radiology suite for transarterial coil embolization. The initial arteriogram was performed using carbon dioxide as the contrast agent. The intraparenchymal pseudoaneurysm was clearly demonstrated with small feeding arteries from proximal hilar branches (Figure C). Selective coil embolization of the feeding upper pole artery branch was performed. Completion angiogram with iodinated contrast demonstrated complete occlusion of the pseudoaneurysm (Figure D).
Discussion
Trauma is the most common cause of splenic rupture. Nontraumatic or spontaneous splenic rupture is rare and most commonly related to massive splenomegaly or anticoagulant/thrombolytic therapy.1,2 Anticoagulant or thrombolytic therapy that causes splenic rupture carries a 24% mortality rate.3 A rare cause of splenic rupture is acute or chronic pancreatitis.1
Splenic intraparenchymal pseudoaneurysm is a complication of spontaneous splenic rupture.4,5 Intraparenchymal pseudoaneurysm may occur in 12% of patients with sonographically detected spontaneous splenic rupture.6
Traumatic or spontaneous rupture is treated with a variety of methods, including splenectomy, transcatheter embolization, or conservative management.5,7 Increasing success rates have shifted endovascular treatment as first-line therapy for splenic injury to conserve splenic function.
— Heather J. Wichman, MD, is in private practice with Milwaukee Radiology in Wisconsin.
— Venkataramu N. Krishnamurthy, MBBS, is an associate professor of radiology at the University of Michigan Health System in Ann Arbor and affiliated with the VA Ann Arbor Healthcare System.
 |
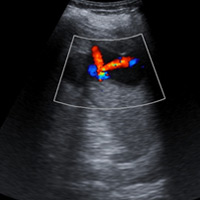 |
| Figure A | Figure B |
 |
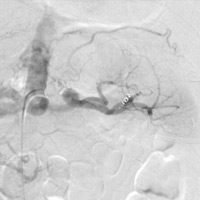 |
| Figure C | Figure D |
Resources
- Habib E, Elhadad A, Slama JL. [Diagnosis and treatment of spleen rupture during pancreatitis.] Gastroenterol Clin Biol. 2000;24(12):1229-1232.
- Görg C, Cölle J, Görg K, Prinz H, Zugmaier G. Spontaneous rupture of the spleen: ultrasound patterns, diagnosis and follow-up. Br J Radiol. 2003;76(910):704-711.
- Blankenship JC, Indeck M. Spontaneous splenic rupture complicating anticoagulant or thrombolytic therapy. Am J Med. 1993;94(4):433-437.
- Hiraide A, Yamamoto H, Yahata K, Yoshioka T, Sugimoto T. Delayed rupture of the spleen caused by an intrasplenic pseudoaneurysm following blunt trauma: case report. J Trauma. 1994;36(5):743-744.
- Sugg SL, Gerndt SJ, Hamilton BJ, Francis IR, Taheri PA, Rodgriguez JL. Pseudoaneurysms of the intraparenchymal splenic artery after blunt abdominal trauma: a complication of nonoperative therapy and its management. J Trauma. 1995;39(3):593-595.
- Görg C, Cölle J, Wied M, Schwerk WB, Zugmaier G. Spontaneous nontraumatic intrasplenic pseudoaneurysm: causes, sonographic diagnosis, and prognosis. J Clin Ultrasound. 2003;31(3):129-134.
- Hagiwara A, Yukioka T, Ohta S, Nitatori T, Matsuda H, Shimazaki S. Nonsurgical management of patients with blunt splenic injury: efficacy of transcatheter arterial embolization. AJR Am J Roentgenol. 1996;167(1):159-166.
Submission Instructions
- Cases should have clinical relevance and clear radiological findings.
- Seconds should include a title, history and course of illness, findings, diagnosis, and discussion.
- Word count should not exceed 800. At least three references are recommended.
- Cases may be submitted from any radiological subspecialty and imaging modality.
- Figures must be high-quality JPEG or TIFF images and labeled for ease of reference. Please keep images in their native format, without the addition of arrows or other means of highlighting the key findings.
Submit cases via e-mail to Rahul V. Pawar, MD, at rvp325@gmail.com or to Radiology Today at jknaub@gvpub.com.
Department of Radiology, Division of Neuroradiology
Saint Barnabas Medical Center/Barnabas Ambulatory Care Center