Web Exclusive
Spectral Detector CT: A Study Among Patients With Renal Insufficiency
By Don Norwood, MD, MBA; Isaac Filat, MA, HSM, CNMT, ARRT (N); Fieke Snijders; and Ekta Dharaiya, MS
With the shift toward value-based care, it's essential for hospitals to improve clinical efficiency and reduce duplication of services to make it easier for patients to get the care they need while managing costs. In value-based models, doctors and hospitals are accountable for treating and improving the health of patients with chronic conditions in a cost-effective way.
Accountable care organizations are transforming care delivery by paying health systems and doctors based on their success at improving overall quality, cost, and patient satisfaction. As a result, physicians and hospitals are continuously looking for tools and technologies to provide quality cost-effective patient care.
Over the last decade, multidetector CT (MDCT) has established its position as the workhorse of radiology. MDCT is used in routine examinations for thoracic, abdominal, pelvic, brain, neck, and spine assessments. With its increasing popularity, about 50% of MDCT examinations are performed with the injection of iodinated contrast, highlighting blood vessels and enhancing organ structure. While the use of iodinated contrast has many benefits, the amount of contrast media delivered to a patient during a CT scan is of utmost concern due to the risk of complications, particularly with contrast-induced nephropathy (CIN).
CIN, the third most common cause of hospital-acquired acute renal failure, produces acute renal failure within 48 hours of exposure to intravascular radiographic contrast material that is not attributable to other causes. Prevention of CIN has been the subject of many discussions; however, due to nonstandardized implementation of contrast management techniques, there has been limited success and varying results across different sites.
Iodinated contrast is imperative to providing clinicians with a better view into their patients, but not all patients can tolerate this contrast. For the contrast to be cleared out of the body, a patient must have normal kidney function. This creates an issue for using contrast with oncology patients and those with renal insufficiency. The types of scans available to these patients will be limited, and because the scans without contrast generally do not give clinicians enough information to make a diagnosis, these patients will have to return for additional scans, with the accompanying additional exposure to radiation.
In an effort to reduce contrast volume in patients with reduced kidney function, a study conducted at CARTI Cancer Center looked to reduce the risk of CIN and provide it with an overall clinical and economic benefit.
Full Contrast Without the Volume
Dual-energy CT scanners have been in clinical use for a few years; however, these scanners are source based with limited dose modulation capabilities, requiring the user to make a decision on whether a patient needs to be scanned in dual-energy mode. The latest innovation in CT detector technology is a spectral detector CT (SDCT) with a single X-ray source and a two-layer detector. From iodine-based results to virtual noncontrast images, spectral imaging has many benefits that can help assist in clinical decision making.
CARTI Cancer Center, a leading outpatient imaging center in Little Rock, Arkansas, installed IQon Spectral Detector CTs in August 2016. Most of its patients are referred for oncology follow-up CT examinations. CARTI would refer all the patients with a high risk of CIN (reduced eGFR) to noncontrast CT scans; these patients would be able to tolerate the volume of contrast that CARTI uses for the contrast-enhanced CT scans for oncology evaluations.
After the SDCT installation, physicians at CARTI realized the benefits of MonoE results and started scanning patients with reduced kidney function using 50 cc to 80 cc of contrast and low MonoE spectral results to boost contrast enhancement in the study. MonoE results is an image that shows attenuation, as if a single monochromatic energy (keV) were used to scan—it can be used to improve iodine signals, contrast to noise, beam-hardening artifact reduction, and metal artifact reduction. This allowed physicians to gain the full benefits of contrast-enhanced exams without using the full volume of contrast.
Study investigators looked at how low MonoE results allow the user to manage the amount of iodinated contrast delivered to the patient. In this study, there were two groups: one containing 30 patients with reduced renal function scanned with noncontrast CT on a MDCT scanner, and the other consisting of patients with reduced renal function scanned with 50 cc to 80 cc of contrast scanned on the SDCT.
Clinicians performed head and neck, and chest/abdomen/pelvis scans in patients with reduced kidney function using a limited amount of iodinated contrast. The patients originally wouldn't have been candidates for a contrast-enhanced CT scan, needing to receive a noncontrast CT, and, depending on the findings, would have required a follow-up scan on another imaging modality such as MRI or ultrasound. The ability to scan these patients with low volumes of contrast helped with the clinical diagnosis and reduced the overall imaging costs by reducing follow-up scans on other modalities.
Spectral CT's Clinical and Economic Impact
Study findings revealed that the 30 patients who received a noncontrast CT would need additional diagnostic tests, including one follow-up MRI and two ultrasound scans within a period of three months. This would result in an additional average cost of $453 in the group of patients using noncontrast CT as compared with those scanned with the SDCT. Also, the need for additional follow-up scanning would add additional time to diagnosis. The use of contrast enhancement on CARTI's SDCT reduced the time to diagnosis of those patients from 100 days to 66 days, a reduction of 34% (this was calculated using the actual exam dates).
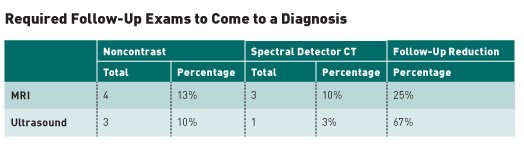
The clinical and economic impact seen at CARTI can be applied to a larger health system. A large health system or integrated diagnostic network (IDN) performs an average of 400,000 total CT scans annually. If 5% of those scans were patients with reduced renal function, that would represent about 20,000 scans. Applying the methodology mentioned above, significant economic benefits can be realized at an IDN level based on the average savings of $453 in the cohort with noncontrast scans, based on the average Medicare reimbursement cost of MRI ($1,109.43) and ultrasound ($124.09).
SDCT's ability to generate spectral results, such as MonoE, enables the scanning of patients with high risk for CIN using iodinated contrast, boosting iodine signal and allowing for improved visualization of structures at low volumes of iodinated contrast. The use of contrast on these patients improves the clinician's ability to identify and delineate lesions and structures in solid organs, thereby reducing the need for additional scanning.
As the health care industry shifts toward a value-based care model, SDCT will continue to gain popularity with clinicians as it allows scanning on an expanded patient population and enables contrast-enhanced scanning on a patient population that would not have been otherwise eligible to receive contrast. By reducing diagnosis time, decreasing the number of follow-up scans, and cutting costs, health care professionals are able to provide patients with the best quality care while improving outcomes.
Results from case studies are not predictive of results in other cases. Results in other cases may vary.
— Don Norwood, MD, MBA, is a staff radiologist at CARTI Cancer Center. Isaac Filat, MA, HSM, CNMT, ARRT (N), is director of imaging at CARTI. Fieke Snijders is CoE lead, health care analytics at Philips Enterprise Information Management. Ekta Dharaiya, MS, is a clinical scientist at Philips Healthcare.
Spectral Detector CT: A Study Among Patients With Renal Insufficiency
By Don Norwood, MD, MBA; Isaac Filat, MA, HSM, CNMT, ARRT (N); Fieke Snijders; and Ekta Dharaiya, MS
With the shift toward value-based care, it's essential for hospitals to improve clinical efficiency and reduce duplication of services to make it easier for patients to get the care they need while managing costs. In value-based models, doctors and hospitals are accountable for treating and improving the health of patients with chronic conditions in a cost-effective way.
Accountable care organizations are transforming care delivery by paying health systems and doctors based on their success at improving overall quality, cost, and patient satisfaction. As a result, physicians and hospitals are continuously looking for tools and technologies to provide quality cost-effective patient care.
Over the last decade, multidetector CT (MDCT) has established its position as the workhorse of radiology. MDCT is used in routine examinations for thoracic, abdominal, pelvic, brain, neck, and spine assessments. With its increasing popularity, about 50% of MDCT examinations are performed with the injection of iodinated contrast, highlighting blood vessels and enhancing organ structure. While the use of iodinated contrast has many benefits, the amount of contrast media delivered to a patient during a CT scan is of utmost concern due to the risk of complications, particularly with contrast-induced nephropathy (CIN).
CIN, the third most common cause of hospital-acquired acute renal failure, produces acute renal failure within 48 hours of exposure to intravascular radiographic contrast material that is not attributable to other causes. Prevention of CIN has been the subject of many discussions; however, due to nonstandardized implementation of contrast management techniques, there has been limited success and varying results across different sites.
Iodinated contrast is imperative to providing clinicians with a better view into their patients, but not all patients can tolerate this contrast. For the contrast to be cleared out of the body, a patient must have normal kidney function. This creates an issue for using contrast with oncology patients and those with renal insufficiency. The types of scans available to these patients will be limited, and because the scans without contrast generally do not give clinicians enough information to make a diagnosis, these patients will have to return for additional scans, with the accompanying additional exposure to radiation.
In an effort to reduce contrast volume in patients with reduced kidney function, a study conducted at CARTI Cancer Center looked to reduce the risk of CIN and provide it with an overall clinical and economic benefit.
Full Contrast Without the Volume
Dual-energy CT scanners have been in clinical use for a few years; however, these scanners are source based with limited dose modulation capabilities, requiring the user to make a decision on whether a patient needs to be scanned in dual-energy mode. The latest innovation in CT detector technology is a spectral detector CT (SDCT) with a single X-ray source and a two-layer detector. From iodine-based results to virtual noncontrast images, spectral imaging has many benefits that can help assist in clinical decision making.
CARTI Cancer Center, a leading outpatient imaging center in Little Rock, Arkansas, installed IQon Spectral Detector CTs in August 2016. Most of its patients are referred for oncology follow-up CT examinations. CARTI would refer all the patients with a high risk of CIN (reduced eGFR) to noncontrast CT scans; these patients would be able to tolerate the volume of contrast that CARTI uses for the contrast-enhanced CT scans for oncology evaluations.
After the SDCT installation, physicians at CARTI realized the benefits of MonoE results and started scanning patients with reduced kidney function using 50 cc to 80 cc of contrast and low MonoE spectral results to boost contrast enhancement in the study. MonoE results is an image that shows attenuation, as if a single monochromatic energy (keV) were used to scan—it can be used to improve iodine signals, contrast to noise, beam-hardening artifact reduction, and metal artifact reduction. This allowed physicians to gain the full benefits of contrast-enhanced exams without using the full volume of contrast.
Study investigators looked at how low MonoE results allow the user to manage the amount of iodinated contrast delivered to the patient. In this study, there were two groups: one containing 30 patients with reduced renal function scanned with noncontrast CT on a MDCT scanner, and the other consisting of patients with reduced renal function scanned with 50 cc to 80 cc of contrast scanned on the SDCT.
Clinicians performed head and neck, and chest/abdomen/pelvis scans in patients with reduced kidney function using a limited amount of iodinated contrast. The patients originally wouldn't have been candidates for a contrast-enhanced CT scan, needing to receive a noncontrast CT, and, depending on the findings, would have required a follow-up scan on another imaging modality such as MRI or ultrasound. The ability to scan these patients with low volumes of contrast helped with the clinical diagnosis and reduced the overall imaging costs by reducing follow-up scans on other modalities.
Spectral CT's Clinical and Economic Impact
Study findings revealed that the 30 patients who received a noncontrast CT would need additional diagnostic tests, including one follow-up MRI and two ultrasound scans within a period of three months. This would result in an additional average cost of $453 in the group of patients using noncontrast CT as compared with those scanned with the SDCT. Also, the need for additional follow-up scanning would add additional time to diagnosis. The use of contrast enhancement on CARTI's SDCT reduced the time to diagnosis of those patients from 100 days to 66 days, a reduction of 34% (this was calculated using the actual exam dates).
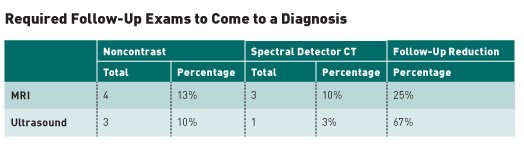
The clinical and economic impact seen at CARTI can be applied to a larger health system. A large health system or integrated diagnostic network (IDN) performs an average of 400,000 total CT scans annually. If 5% of those scans were patients with reduced renal function, that would represent about 20,000 scans. Applying the methodology mentioned above, significant economic benefits can be realized at an IDN level based on the average savings of $453 in the cohort with noncontrast scans, based on the average Medicare reimbursement cost of MRI ($1,109.43) and ultrasound ($124.09).
SDCT's ability to generate spectral results, such as MonoE, enables the scanning of patients with high risk for CIN using iodinated contrast, boosting iodine signal and allowing for improved visualization of structures at low volumes of iodinated contrast. The use of contrast on these patients improves the clinician's ability to identify and delineate lesions and structures in solid organs, thereby reducing the need for additional scanning.
As the health care industry shifts toward a value-based care model, SDCT will continue to gain popularity with clinicians as it allows scanning on an expanded patient population and enables contrast-enhanced scanning on a patient population that would not have been otherwise eligible to receive contrast. By reducing diagnosis time, decreasing the number of follow-up scans, and cutting costs, health care professionals are able to provide patients with the best quality care while improving outcomes.
Results from case studies are not predictive of results in other cases. Results in other cases may vary.
— Don Norwood, MD, MBA, is a staff radiologist at CARTI Cancer Center. Isaac Filat, MA, HSM, CNMT, ARRT (N), is director of imaging at CARTI. Fieke Snijders is CoE lead, health care analytics at Philips Enterprise Information Management. Ekta Dharaiya, MS, is a clinical scientist at Philips Healthcare.

