 On the Case
On the Case
By Daniel Chen, MD, and Alex Merkulov, MD
Radiology Today
Vol. 21 No. 1 P. 30
History
A 34-year-old woman underwent a complicated C-section secondary to HELLP syndrome, characterized by hemolysis, elevated liver enzymes, and a low platelet count. She had postpartum right upper quadrant (RUQ) abdominal pain and hypertension. An ultrasound was done to evaluate the RUQ and for renal artery stenosis. On ultrasound, a cystic liver mass was identified adjacent to the gallbladder. CT was ordered to further characterize the liver, and the patient was referred to general surgery for an evaluation.
Findings
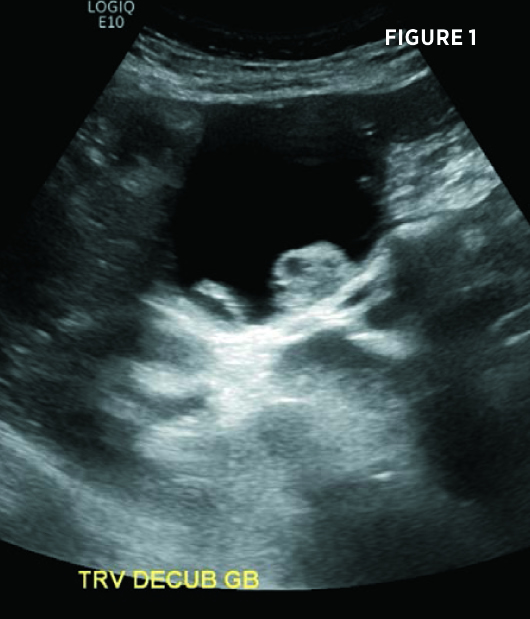
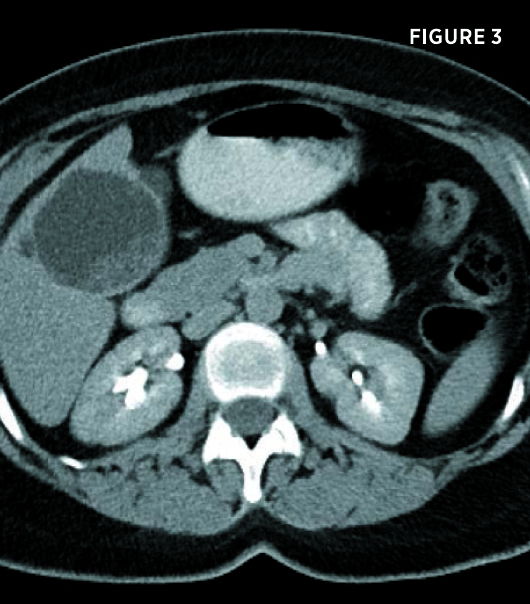
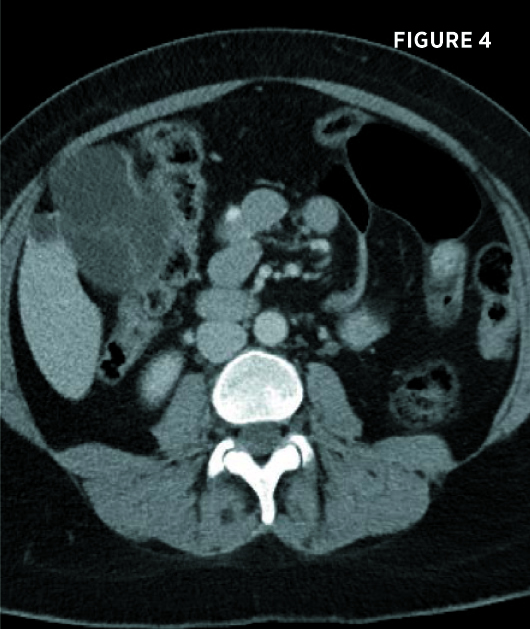
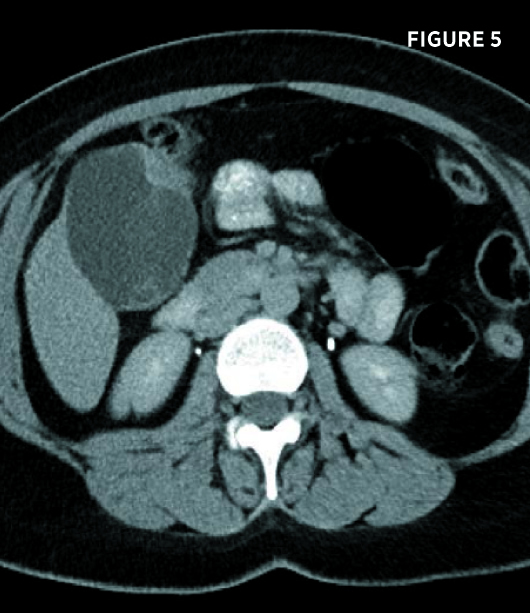
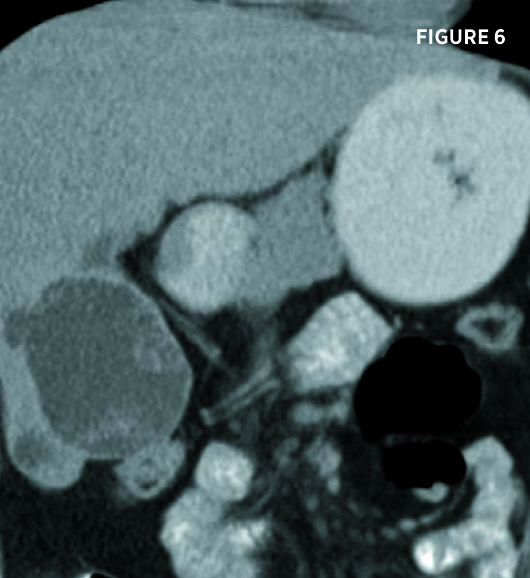
Transverse and longitudinal ultrasound images (Figures 1 and 2) demonstrate a multiseptated cystic liver mass, centered posteriorly to the gallbladder, with mural nodules and enhanced through transmission. Axial and coronal contrast-enhanced CT images demonstrate a 7.3-cm segment IV left hepatic lobe cystic mass abutting the gallbladder. The mass contained mildly enhancing septations and enhancing peripheral mural nodules (Figures 3, 4, 5, and 6). There was no intra- or extrahepatic biliary ductal dilatation.
The patient was subsequently evaluated by general surgery. Given the complex morphology of the cystic liver mass, it was recommended to the patient to proceed with cystic mass fenestration, with an intraoperative frozen section examination, as well as cholecystectomy, given the location of the hepatic cyst and her RUQ pain. The patient underwent an uncomplicated laparoscopic hepatic cyst fenestration and cholecystectomy.

Diagnosis
Biliary mucinous cystadenoma.
Discussion
Biliary cystadenomas are a rare family of benign but premalignant cystic neoplasms of the biliary ductal system. The reported incidence of biliary cystadenomas is 1 in 100,000 to 5 in 100,000, with a reported risk of malignant transformation as high as 20%. An estimated 85% to 95% of cases occur in white women, with peak incidence between the ages of 55 and 65. The majority of these tumors (80% to 85%) arise in the liver, with a minority arising in extrahepatic bile ducts and a few case reports of tumors arising in the gallbladder.
The etiology of biliary cystadenomas is not fully understood. Current theories suggest that the neoplasms may originate from primitive hepatobiliary stem cells or congenitally aberrant biliary ducts. The fact that tumors arise almost exclusively in women, as well as reports of increased incidence in oral contraceptive users, suggests that these tumors may be estrogen sensitive.
While small biliary cystadenomas are frequently asymptomatic, typical presentation for larger tumors include gradually increasing abdominal pain and/or swelling, increase in abdominal girth, or a palpable mass. Less commonly, these lesions may cause gastrointestinal obstruction, nausea, vomiting, dyspepsia, anorexia, or ascites. Rarely cystic rupture, intracystic hemorrhage, or secondary infection may occur. Cases of vascular obstruction, particularly of the inferior vena cava, have also been reported.
Radiologically, differential diagnosis includes simple liver cysts; infectious cysts, ie, hydatid cysts; traumatic cysts; an abscess; metastatic lesions from ovarian or pancreatic adenocarcinoma; primary tumors such as biliary cystadenocarcinoma; cystic cholangiocarcinoma; cystic primary hepatocellular carcinoma; and hepatobiliary mesenchymal tumors. Of these lesions, the classic radiologic appearance of biliary cystadenoma is most easily confused with hydatid cysts; therefore, special attention should be paid to patient history and presenting symptoms in differentiating these lesions. Additionally, biliary cystadenoma and biliary cystadenocarcinoma cannot be reliably differentiated by radiologic or physical appearance; pathological analysis is required.
Biliary cystadenoma may be visualized on abdominal ultrasound, CT, or MRI. Typical appearance on ultrasound, which is commonly used for initial investigation, is a thick-walled, well-demarcated globular or ovoid, predominantly anechoic, mass with thin, highly echogenic internal septations. Tumors may demonstrate internal Doppler vascular flow.
On CT, biliary cystadenomas are usually well-demarcated, internal low-density lobulated cystic lesions with contrast-enhancing walls and septations. Associated intra- or extrahepatic biliary dilation may also be seen.
On MRI, these lesions appear similar in morphology, although internal signal intensity may vary depending on the protein content and presence or absence of internal hemorrhage. Typically, these lesions demonstrate homogenous low-intensity T1 signal and high-intensity T2 signal consistent with internal simple fluid. In any modality, imaging findings that suggest malignancy—biliary cystadenocarcinoma—include irregular wall thickness, mural nodules, and vascular papillary projections.
These lesions are typically managed with surgical resection. Due to the relatively high risk for malignant transformation, surgery is indicated, even for asymptomatic patients. With incomplete resection, fenestration, intratumoral sclerosant application, fulguration, or drainage, recurrence is expected. With complete removal, such as with enucleation, hepatic wedge resection, or lobectomy, prognosis is excellent with very rare recurrence.
— Daniel Chen, MD, is a radiology resident at UConn Health at the University of Connecticut.
— Alex Merkulov, MD, is an associate professor of radiology at UConn Health.
Resources
1. Tsepelaki A, Kirkilesis I, Katsiva V, Triantafillidis JK, Vagianos C. Biliary cystadenoma of the liver: case report and systematic review of the literature. Ann Gastroenterol. 2009;22(4):278-283.
2. Rooney TB, Schofer JM, Stanley MD, Banks SL. Biliary cystadenoma of the gallbladder. AJR Am J Roentgenol. 2005;185(6):1571-1572.
3. Soares KC, Arnaoutakis DJ, Kamel I, et al. Cystic neoplasms of the liver: biliary cystadenoma and cystadenocarcinoma. J Am Coll Surg. 2014;218(1):119-128.

