 On the Case
On the Case
By Thomas Wilczynski, DO; Anne Misiura, MD; and Laurence J. Spitzer, MD
Radiology Today
Vol. 20 No. 2 P. 30
History
A 35-year-old gravida 4, para 4 woman with no significant past medical history presented for evaluation of a lost string from an intrauterine device (IUD) placed the month prior. Pelvic ultrasound imaging revealed a nonspecific 1 mm linear echogenicity in the posterior cul-de-sac, but no IUD within the uterus. Abdominal and pelvic radiography was then ordered.
Findings
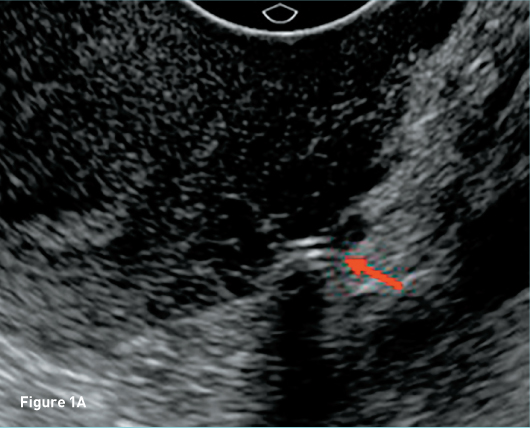
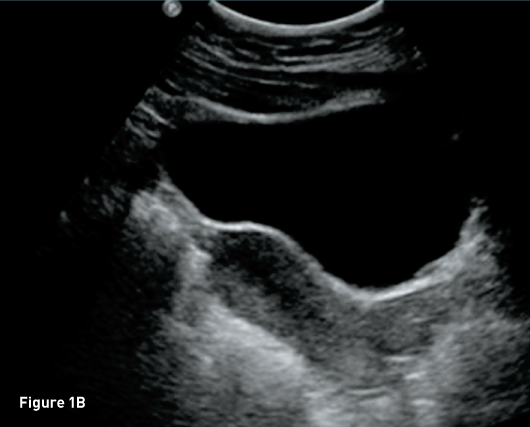
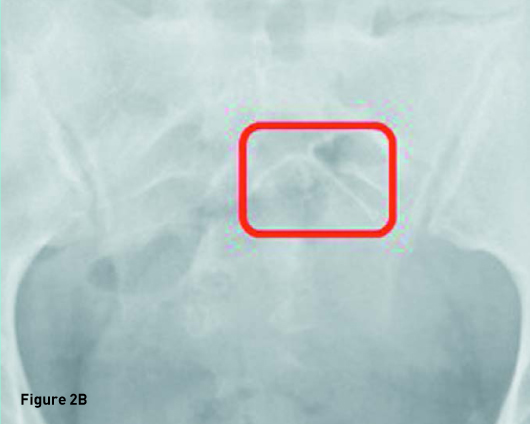
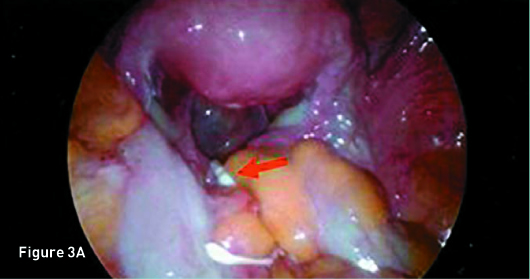
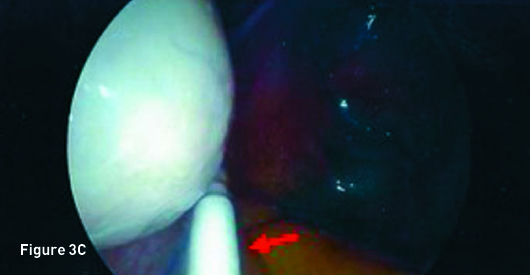
Transverse transvaginal gray scale ultrasound image demonstrates a 1 mm linear nonspecific echogenicity in the posterior cul-de-sac (red arrow) and no IUD (Figure 1A). Sagittal transabdominal ultrasound image demonstrates a morphologically normal uterus (Figure 1B). Abdominal (Figure 2A) and pelvic (Figure 2B) radiographs demonstrate a T-shaped IUD overlying the left sacrum. A laparoscopic procedure was performed to remove the extrauterine IUD and confirmed perforation of the uterine fundus. Laparoscopic images from the operating room confirm the T-shaped IUD located in the posterior cul-de-sac with a small amount of adjacent free fluid (Figures 3A, 3B, and 3C).


Diagnosis
Migration of an IUD secondary to complete uterine perforation.
Discussion
IUDs are a frequently used form of temporary female contraception. The most common IUDs are T-shaped and contain hormones (levonorgestrel) or copper to create a hostile environment for pregnancy implantation. Correctly positioned IUDs should be located in the endometrial canal at the uterine fundus with the side arms extending toward the cornua and the stem extending into the uterine body.1,2 The role of the radiologist in IUD imaging is to confirm correct IUD positioning, which is crucial for both contraceptive efficacy and patient safety.2
Migration of IUDs includes expulsion, intrauterine displacement, embedment, or the rarest complication, uterine perforation.3 Complete uterine perforation, in which the IUD penetrates all three uterine layers and is either partially or completely intraperitoneal is the most serious complication, as it may lead to additional morbidity in the form of injury to nearby structures (eg, bowel perforation), adhesions, intra-abdominal infection, or abscess.
In evaluation of malpositioned IUDs, ultrasonography is the imaging modality of choice after clinical evaluation has failed to locate a "missing string." If ultrasonography fails to identify the IUD, plain radiographs of the abdomen and pelvis are typically warranted. Although CT is not the first line, in the emergent setting, CT imaging is commonly used as the initial imaging modality and as a means to exclude other causes of pelvic pain.
Occurring in a documented 1 in 1,000 cases, uterine perforation is believed to be related to low estrogen levels resulting in uterine shrinkage with a possible component of other uterine abnormalities and/or clinical inexperience.4 When a "lost string" is the clinical indication bringing the patient to the radiology department, accurate detection/localization of the IUD by the radiologist is paramount, as management of an intraperitoneal IUD entails urgent laparoscopy or laparotomy for removal and exploration of adjacent structures.
— Thomas Wilczynski, DO, is a radiologist in the department of radiology at Hahnemann University Hospital of Drexel University College of Medicine in Philadelphia.
— Anne Misiura, MD, is a radiologist in the department of radiology at Hahnemann University Hospital of Drexel University College of Medicine.
— Laurence J. Spitzer, MD, is an assistant professor of radiology in the department of radiology at Hahnemann University Hospital of Drexel University College of Medicine.
References
1. Braaten, KP, Goldberg AB. Malpositioned IUDs: when you should intervene (and when you should not). OBG Manag. 2012;24(8):38-46.
2. Nowitzki KM, Hoimes ML, Chen B, Zheng LZ, Kim YH. Ultrasonography of intrauterine devices. Ultrasonography. 2015;34(3):183-194.
3. Mausner EV, Yitta S, Slywotzky CM, Bennett GL. Commonly encountered foreign bodies and devices in the female pelvis: MDCT appearances. AJR Am J Roentgenol. 2011;196(4):W461-W470.
4. Boortz HE, Margolis DJ, Ragavendra N, Patel MK, Kadell BM. Migration of intrauterine devices: radiologic findings and implications for patient care. Radiographics. 2012;32(2):335-352.

