 On the Case
On the Case
By Kathryn Becker, MD, and Alex Merkulov, MD
Radiology Today
Vol. 22 No. 2 P. 30
History
A 29-year-old man presented to the emergency department (ED) with a three-day history of persistent headache. The patient also reported chills, dizziness, and two episodes of vomiting. He was up to date on vaccines, worked in landscaping, and was not taking any medications. He denied a tick bite. At that time, labs were drawn, including a tick panel. The patient was discharged home with doxycycline for presumed ehrlichiosis.
Three days later, the patient returned to the ED with a 9/10 in intensity—on a 0 to 10 pain scale—constant, bifrontal, pulsationlike headache which was associated with sensitivity to light and nausea. He denied focal numbness, weakness, change in mental status, confusion, or lightheadedness. Upon physical exam, the patient was afebrile, appeared nontoxic, had no clinical signs of meningitis, and had a normal neurologic exam. CT imaging of the brain was ordered. The patient subsequently underwent an MR venogram (MRV) of the brain without and with IV contrast and an MRI of the brain without IV contrast.
Findings
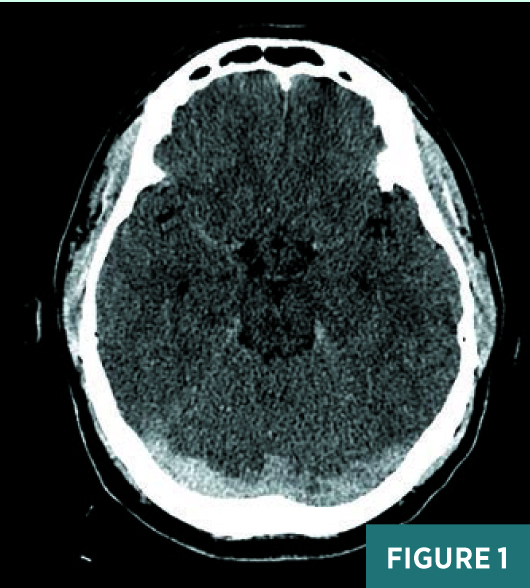
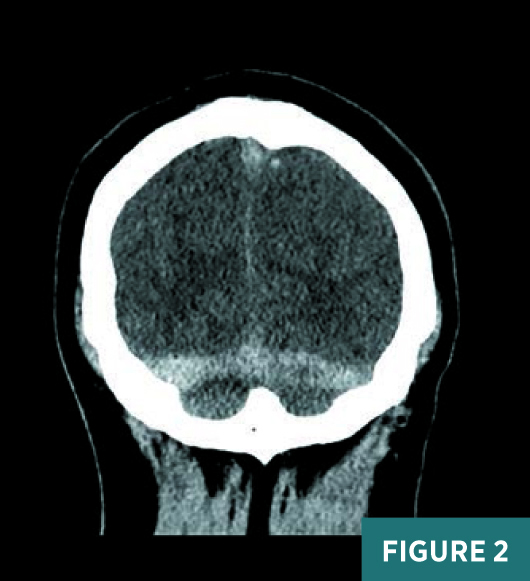
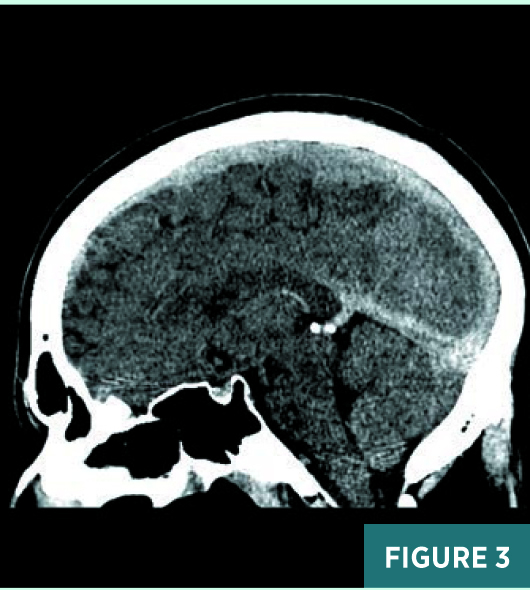
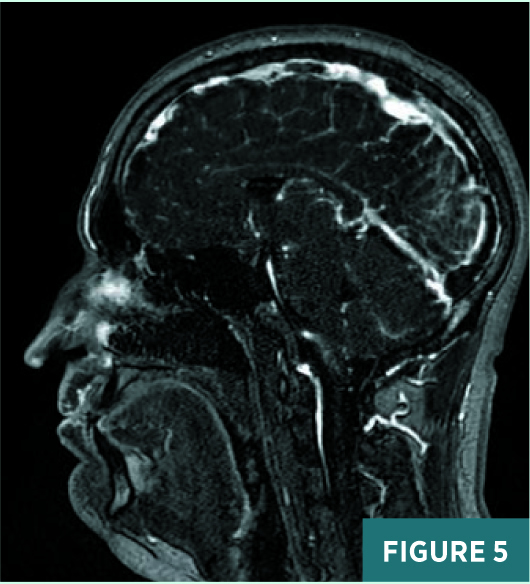
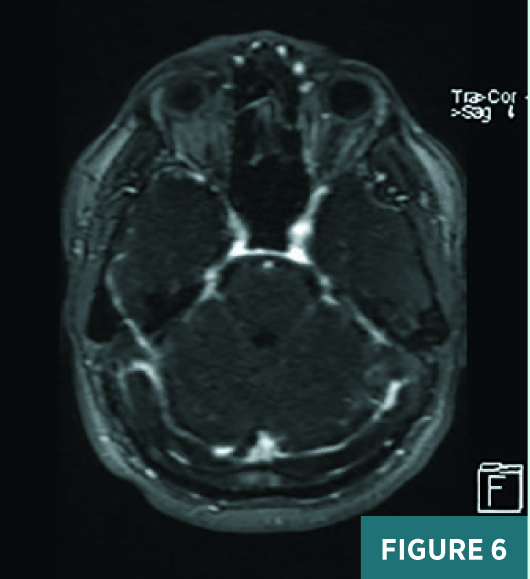
Axial, coronal, and sagittal nonenhanced CT images demonstrated areas of abnormal prominence and hyperattenuation involving the superior sagittal sinus, vein of Galen, straight sinus, and transverse sinuses consistent with cerebral venous sinus thrombosis, or CVST (Figures 1-3). On CT, the transverse sinuses measured 69 Hounsfield units (HU) in density, in reference to the middle cerebral artery density of 40 HU. MRV 2D time-of-flight (TOF) maximum intensity projection, T1 3D volumetric interpolated breath-hold examination (VIBE) sagittal post-contrast fat saturation, and 1 mm multiplanar reformation axial postcontrast sequences (Figures 4-6) confirmed extensive CVST involving the superior sagittal sinus, vein of Galen, and straight bilateral transverse and bilateral sigmoid sinuses. MRI of the brain excluded venous infarction or additional intracranial abnormalities.
The patient was then evaluated by neurology and neurosurgery, admitted to the ICU, started on a heparin drip, and subsequently switched to Lovenox during his hospital stay. Hematology, infectious disease, and ophthalmology were consulted during the patient’s hospital stay. Blood cultures and infectious panel were negative, including tests for HIV and tick-borne illnesses. Although concern for infectious etiology persisted, particularly as the patient developed a transient fever during his stay, a lumbar puncture was not performed, due to increased intracranial pressure and increased risk of subsequent herniation. Eventually, the hypercoagulability workup revealed both a methylenetetrahydrofolate reductase mutation and prothrombin gene mutation.
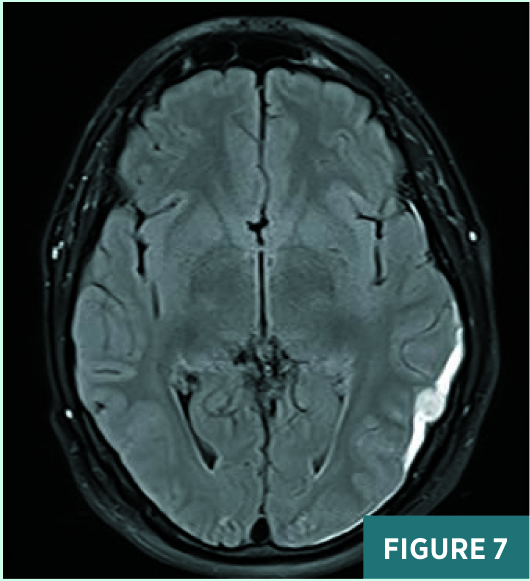
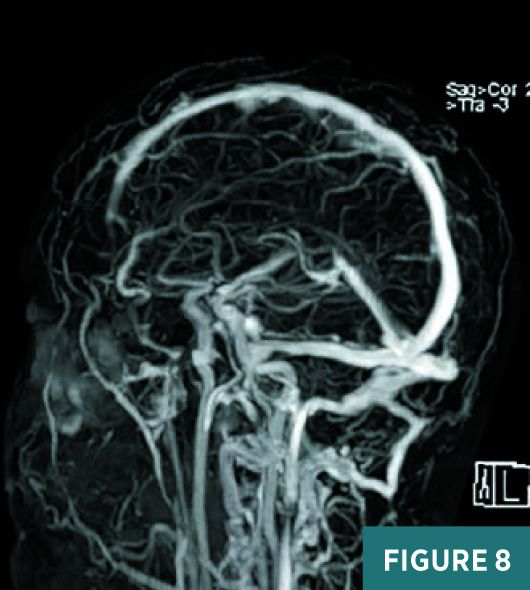
Upon discharge, the patient continued to have headaches and noted blurred vision in the right eye. An outpatient ophthalmology appointment revealed papilledema, which subsequently worsened on follow-up visits. Diamox/Lasix dose was increased. The patient had a follow-up MRI and MRV five weeks after discharge. MRI revealed a small late subacute left occipitotemporal subdural hematoma, on axial FLAIR sequence (Figure 7), which completely resolved on follow-up imaging. MRV demonstrated complete interval recanalization of the previously thrombosed sinuses and no evidence of residual CVST, on MRV tumble postcontrast image (Figure 8).
After six months of follow-up, the papilledema resolved. Patient will continue on lifelong anticoagulation therapy.
Diagnosis
CVST.

Discussion
Headache is one of the most common patient presentations in the ED. Clinical signs, symptoms, and types of headache are associated with increased likelihood of a serious intracranial abnormality. These include an abnormal neurologic exam, a cluster-type headache, the patient seeing an aura or vomiting, and a headache aggravated by exertion or Valsalva maneuver. Other relevant clinical information includes pain radiating to the face or neck, Horner syndrome, cranial nerve palsy, fever, immunosuppression, known malignancy or HIV infection, pregnancy, vision loss, or pulsatile tinnitus.
A thunderclap headache is a special consideration. This is a severe headache with a pain score of 7 or greater (0 to 10 pain scale), with pain peaking within seconds or minutes of onset. Differential considerations for a thunderclap headache include subarachnoid hemorrhage, ruptured cerebral aneurysm or reversible cerebral vasoconstriction syndrome, intracranial hypertension and hypotension, infection, cervical artery dissection, CVST, or pituitary apoplexy.
Dural venous sinuses drain the central nervous system, face, and scalp. They lack valves and, ultimately, drain into the internal jugular veins. The straight, superior, and inferior sagittal sinuses converge at the confluence of sinuses. The straight sinus is a continuation of the great cerebral vein (vein of Galen) and the inferior sagittal sinus. From the confluence, the transverse sinus continues bilaterally and curves into the sigmoid sinus to meet the opening of the internal jugular vein. The cavernous sinus drains the ophthalmic veins and is found on either side of the sella turcica. From here, the blood returns to the internal jugular vein via the superior or inferior petrosal sinuses.
CVST is relatively rare. It is characterized by the presence of a thrombus within the dural venous sinuses, which occludes venous return, causes an accumulation of deoxygenated blood within the brain parenchyma, and can lead to a venous infarction. The situation is further complicated by an accumulation of cerebrospinal fluid and subsequent increase in the intracranial pressure, causing papilledema and altered mental status.
Almost all patients with CVST present with a headache, which tends to worsen over a period of several days but may also develop suddenly, eg, thunderclap headache. Patients may also present with focal neurologic deficits and seizures, which is most common in women who are peripartum. Focal neurologic symptoms are often seen in those patients with parenchymal changes on imaging.
CVST is more common in particular situations. Eighty-five percent of patients have at least one of the following risk factors: thrombophilia, eg, factor V Leiden or deficiency of protein C, protein S, or antithrombin; pregnant or in peripartum state; use oral contraceptives; nephrotic syndrome; chronic inflammatory disease, eg, irritable bowel syndrome or systemic lupus erythematosus; meningitis, mastoiditis, or sinusitis; polycythemia vera and paroxysmal nocturnal hemoglobinuria; homocystinuria; dehydration; or trauma.
Imaging plays an important role in diagnosis of CVST. Nonenhanced CT of the brain classically shows increased attenuation in the sinuses. However, other entities can cause the sinuses to appear hyperdense, including elevated hemoglobin or hematocrit. On noncontrast MRI, CVST manifests by the lack of the normal flow void with abnormal signal in the affected sinus.
Contrast-enhanced CT or MR will demonstrate intraluminal filling defects within the affected sinuses. As in all imaging of blood on MRI, the signal intensity will vary depending on the age of the clot. On contrast-enhanced studies, the classic empty delta sign appears as a triangular filling defect in the superior sagittal sinus. TOF and contrast-enhanced MRV and CT venography are highly useful in diagnosis. On gadolinium-enhanced imaging, contrast enhancement of a chronic thrombus may be seen, secondary to vascularization, collateral vessels within and surrounding the thrombus, and slow flow. This enhancement may serve as a source of confusion, as the appearance is similar to the normal sinus enhancement.
Secondary findings of venous sinus thrombosis include cerebral edema, hemorrhage, and intracranial hypertension. Venous hypertension can result in vasogenic edema, which will not generally show findings on diffusion imaging. Parenchymal changes related to cytotoxic edema will demonstrate restricted diffusion. Lobar hemorrhages are seen in as many as one-third of cases.
The treatment for CVST is anticoagulation, even in the setting of associated intracranial hemorrhage. Cerebral herniation is the most common cause of death in patients, and they should be monitored closely for evidence of increasing intracranial pressure and impending herniation. Intravascular intervention or decompressive craniectomy may be warranted in certain cases in which patients experience worsening symptoms or deterioration.
— Kathryn Becker, MD, is a radiology resident at UConn Health at the University of Connecticut.
— Alex Merkulov, MD, is an associate professor of radiology at UConn Health.
Resources
1. Black DF, Rad AE, Gray LA, Campeau NG, Kallmes DF. Cerebral venous sinus density on noncontrast CT correlates with hematocrit. AJNR Am J Neuroradiol. 2011;32(7):1354-1357.
2. Leach JL, Fortuna RB, Jones BV, Gaskill-Shipley MF. Imaging of cerebral venous thrombosis: current techniques, spectrum of findings, and diagnostic pitfalls. Radiographics. 2006;26(Suppl 1): S19-S41.
3. Luo Y, Tian X, Wang X. Diagnosis and treatment of cerebral venous thrombosis: a review. Front Aging Neurosci. 2018;10:2.
4. Provenzale JM, Kranz PG. Dural sinus thrombosis: sources of error in image interpretation. AJR Am J Roentgenol. 2011;196(1):23-31.

