 May 2016
May 2016
Radiology Billing and Coding: It's All in Your Head
By Melody W. Mulaik, MSHS, CRA, FAHRA, RCC, CPC, CPC-H
Radiology Today
Vol. 15 No. 7 P. 6
Over the last few years, the neurointerventional subspecialty has undergone a significant number of coding changes that have had an overall negative impact on reimbursement. When new codes are created specifically for neurointerventional services, this usually creates excitement and apprehension at the same time. It is always a good thing to have a code that accurately describes a complex service, as long as the corresponding reimbursement is present. This article will focus on the new intracranial codes effective January 1, 2016, to assist with ensuring accurate and compliant coding and billing practices.
For 2016, many existing interventional procedure codes were revised to specifically exclude percutaneous intracranial procedures, and new codes were created to define these services. For example, the arterial thrombectomy codes (37184 to 37186) were revised to indicate they are not to be used for intracranial procedures. Additionally, procedure code 37211 for thrombolysis was revised to indicate that it should not be used for intracranial infusions. There is a cross-reference in the CPT Manual to 61645 for intracranial arterial mechanical thrombectomy and/or thrombolytic infusion.
One new code (61645) has been established for intracranial percutaneous arterial mechanical thrombectomy and/or infusion, and two codes (61650 and 61651) have been established for arterial intracranial prolonged administration of pharmacologic agent(s) other than for thrombolysis. These codes include selective catheterization; diagnostic angiography and all subsequent angiography within the vascular territory; radiological supervision and interpretation (S&I) and fluoroscopic guidance; neurologic and hemodynamic monitoring; and arteriotomy closure by pressure, closure device, or suture. Note that these codes are specifically for arterial treatment and should not be assigned for treatment of intracranial veins.
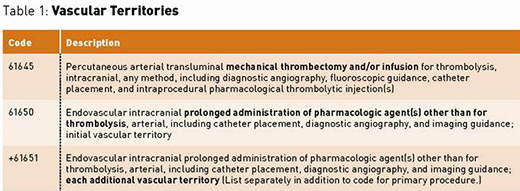
Vascular Territories
The codes can be assigned only once per vascular territory, and there are three intracranial vascular territories: right carotid circulation, left carotid circulation, and vertebro-basilar circulation. The specific vessels in the vascular territories are recognized, as shown in the following table:
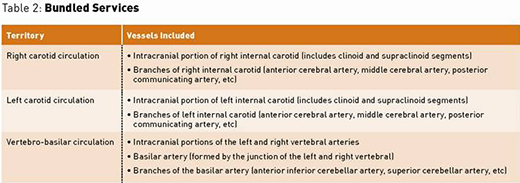
Bundled Services
All three of these codes include the following services except for the one noted exception for each code:
• selective catheterization within the treated vascular territory;
• diagnostic angiography (including 36221 to 36226 and 36228) within the treated vascular territory;
• all subsequent angiography and radiological S&I within the treated vascular territory;
• 61645 only: balloon angioplasty (61630) or stenting (61635) within the treated territory;
• 61650 & 61651 only: balloon dilation (procedures represented by 61640 to 61642);
• fluoroscopic guidance;
• neurologic and hemodynamic monitoring; and
• arteriotomy closure by pressure, closure device, or suture.
Arteriograms in nontreated vascular territories can be reported separately. For example, if the intervention involves the right carotid territory, diagnostic arteriograms of the left carotid and/or vertebral artery can be reported separately.
Intracranial Thrombectomy/Thombolysis (61645)
Code 61645 represents endovascular revascularization of intracranial arteries that are occluded by thrombosis or embolism. This procedure code is covered (status A) under the Medicare Physician Fee Schedule (MPFS). The 2016 Final Rule for the Medicare Outpatient Prospective Payment System indicates code 61645 is status E (not paid by Medicare when submitted on outpatient claims).
This code can be used for any method of thrombectomy/thrombolysis, such as the following:
• Mechanical thrombectomy with a retrieval device like a stentriever (retrievable stent) or an aspiration catheter. Examples of stentrievers include the Trevo and Solitaire devices. The MERCI device is not a stentriever but is also classified as a mechanical retrieval device. The Penumbra System is an example of an aspiration device.
• Administration of "any agent(s) for the purpose of revascularization," including tissue plasminogen activator and other thrombolytic drugs as well as glycoprotein IIb/IIIa inhibitors like ReoPro (abciximab) and Integrilin (tirofiban).
Code 61645 should not be reported together with the following procedures unless performed in different vascular territories:
• peripheral arterial mechanical thrombectomy (37184, 37186);
• prolonged intracranial administration of nonthrombolytic agents (61650, 61651); and
• intracranial angioplasty (61630) or stent placement (61635).
EXAMPLE: A patient presents with an acute stroke. Via femoral access, the left and right internal carotid arteries are catheterized and intracranial arteriograms performed. The patient is found to have thrombosis of the left middle cerebral artery (MCA). The MCA is catheterized, and another angiogram is performed. Then the physician uses a stentriever to remove the clot. Completion angiograms reveal significant restoration of flow.
CODE: 61645 (thrombectomy), 36224-59* (right intracranial carotid arteriogram)
Code 61645 includes the left-sided carotid and MCA catheterizations and arteriograms as well as the clot retrieval. The right-sided carotid arteriogram is coded separately.
*Individual payer guidelines may direct you to use modifier XS or XU.
Prolonged Intracranial Nonthrombolytic Administration (61650 and 61651)
Physicians may perform intracranial transcatheter drug administration for purposes other than thrombolysis. Examples include administration of papaverine to treat vasospasm and administration of vasopressin to constrict a bleeding vessel. The two new codes, 61650 and 61651, can be used for prolonged intracranial administration of chemotherapy drugs or of spasmolytic drugs like papaverine and verapamil. These codes are covered (status A) under the MPFS. They are designated as inpatient-only procedures (status C) under the Hospital Outpatient Prospective Payment System.
The CPT Manual states that codes 61650 and 61651 should not be used for administration of substances that are routinely given during endovascular procedures, such as heparin, nitroglycerin, and saline solution. Rather, these codes represent services to treat "noniatrogenic central nervous system diseases or sequelae thereof." This means these codes should not be assigned when intracranial drug administration is performed to treat vasospasm or other complications caused by a procedure such as carotid angiography or carotid stenting.
The codes are assigned per territory, as previously defined. If more than one territory is treated, code 61650 is assigned for the first territory and 61651 is assigned for each additional territory. Because only three territories are recognized, no more than two units of add-on code 61651 can be reported per day. There must be at least 10 minutes of documented drug administration in each territory coded. Discontinuous blocks of time may be added together. For example, if the physician administers a spasmolytic drug into the right MCA over a period of seven minutes and later administers an additional quantity over a period of five minutes, code 61650 can be reported since the total administration time is 12 minutes. Alternatively, neither code 61650 nor 61651 can be assigned if the patient receives six minutes of drug administration in the right carotid territory and six minutes in the left carotid territory, since the patient did not receive 10 minutes of drug administration in any one territory.
Codes 61650 and 61651 should not be reported together with the following procedures unless performed in different vascular territories:
• balloon dilation of intracranial vasospasm (61640 to 61642);
• peripheral arterial mechanical thrombectomy (37184, 37186);
• intracranial thrombectomy/thrombolysis (61645); and
• intra-arterial chemotherapy (96420, 96422, 96423, 96425).
EXAMPLE: A patient develops vasospasm following subarachnoid hemorrhage. Via femoral access, the physician advances a catheter into the distal left internal carotid artery. Intracranial arteriogram reveals marked vasospasm of the internal carotid and its branches. Papaverine is then administered intermittently over a 20-minute period with a total administration time of 12 minutes. Completion angiogram reveals marked improvement in vessel diameter.
CODE: 61650 (prolonged nonthrombolytic administration)
Remember that code 61650 includes the right carotid catheterizations and arteriograms as well as the papaverine administration.
Summary
The biggest challenge with the new neurointerventional codes is to ensure that the services are not inappropriately unbundled and, conversely, that appropriate charges are not inadvertently omitted, thus causing a loss of precious revenue. It is important that you discuss these new codes with the neurointerventionalists to ensure that they are aware of the rules associated with each code so that appropriate documentation is present.
— Melody W. Mulaik, MSHS, CRA, FAHRA, RCC, CPC, CPC-H, is president and cofounder of Coding Strategies, which provides specialty-specific auditing and educational services for physicians, hospitals, and billing companies nationwide.

