 On the Case
On the Case
By Michelle J. Romero, MD; Swapnil Bagade, MD; and Alex Merkulov, MD
Radiology Today
Vol. 21 No. 5 P. 30
History
A 56-year-old man with a past medical history significant for asthma, depression/anxiety, gastroesophageal reflux disease, gout, type 2 diabetes mellitus, and obstructive sleep apnea presented to the emergency department (ED) and reported a several-week history of nonproductive dry cough, along with fevers in the 101° F to 102° F range. He also reported a loss of appetite with associated weight loss and gastroenteritis-like symptoms with mild diarrhea. He initially went to his primary care physician and was started on a Zithromax Z-Pak. Subsequently, the patient remained self-quarantined with his wife, who was also “sick.” She had a cough and difficulty sleeping. After the patient’s symptoms did not improve, he was referred to the ED. The patient denied dyspnea or any recent travel. On physical exam, the patient was mildly tachycardic, tachypneic, and had a low-grade fever. He was admitted to the hospital and placed in isolation as well as on contact, droplet, and airborne precautions. He subsequently underwent a CT of the chest with IV contrast.
Findings
Axial and coronal chest CT images in lung windows demonstrate multiple bilateral, predominantly subpleural, ground-glass opacities (GGO) and airspace consolidations (Figures 1–6). These nonspecific CT imaging findings mimicked those of atypical or organizing pneumonia. On admission, the patient was considered septic with a positive source for infection, based on his chest CT. The patient received Rocephin and azithromycin, and two sets of blood cultures were sent. The patient was also started on Tamiflu until influenza was ruled out and Tamiflu was discontinued. Additionally, the patient was started on hydroxychloroquine, and two days later his test came back positive for COVID-19. The patient continued to improve clinically. After a six-day hospital admission, the patient was discharged home on oral antibiotics and advised to remain quarantined for 14 days.
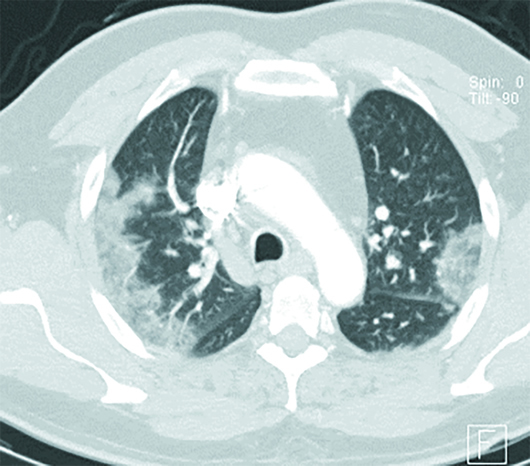
Figure 1
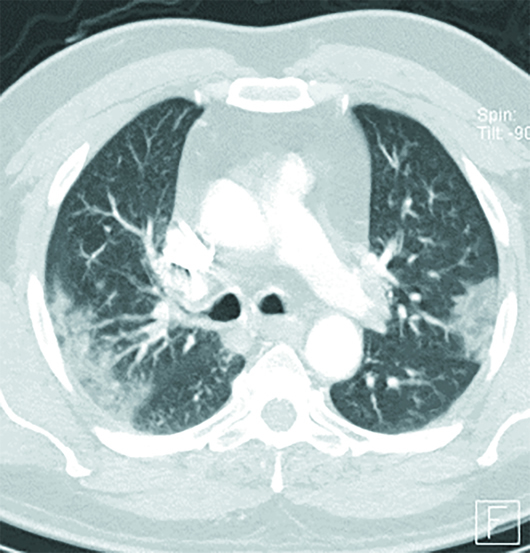
Figure 2
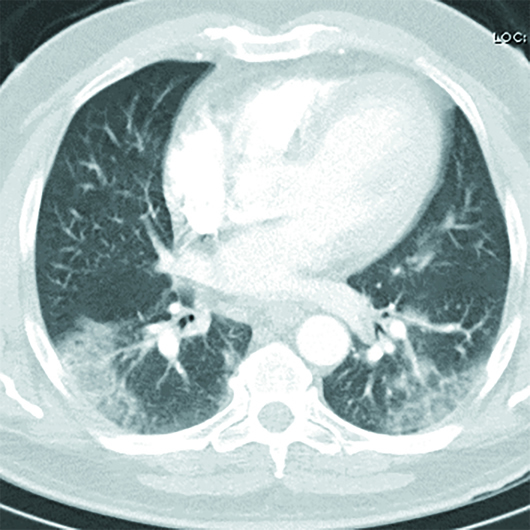
Figure 3
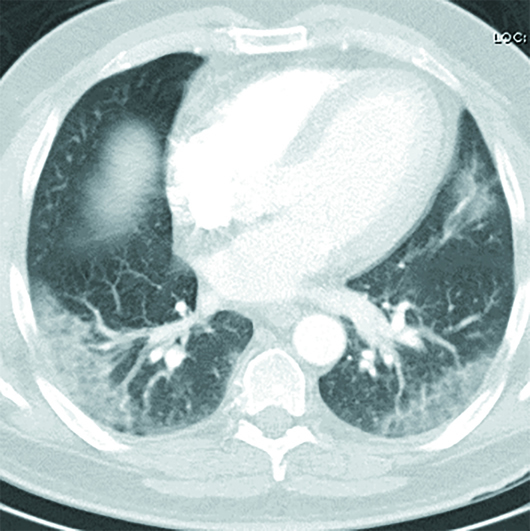
Figure 4
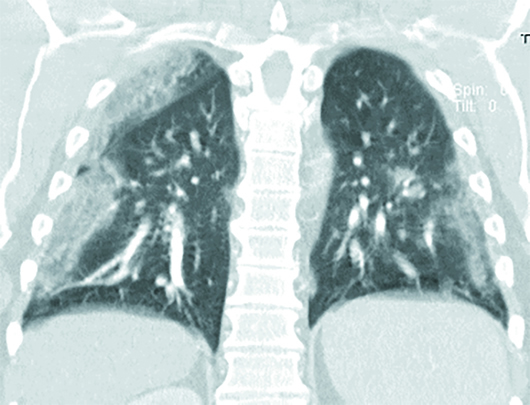
Figure 5
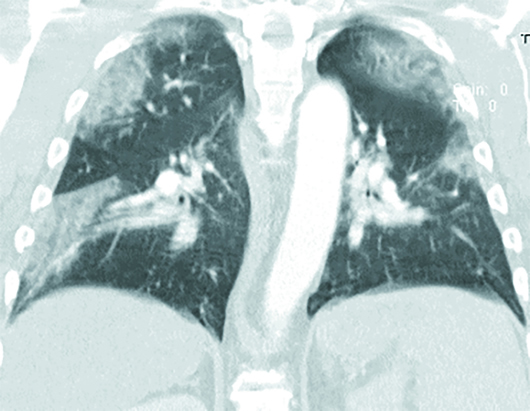
Figure 6
Diagnosis
COVID-19 pneumonia.
Discussion
COVID-19 is an infectious disease caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2). Human coronaviruses are enveloped, single-stranded, RNA viruses that affect humans, mammals, and birds, causing both acute and chronic illnesses of the pulmonary, central nervous system, and gastro-hepatic systems.
The first coronavirus was identified in 1966 in patients with the common cold. Four of the seven known human coronaviruses (HKU1, NL63, OC43, and 229E) cause mild acute upper respiratory inflammatory contagious disease. There are three significantly more virulent zoonotic strains of coronavirus (SARS-CoV, MERS-CoV, and the novel SARS-CoV-2), which may sometimes be fatal. The genome of SARS-CoV-2 has an 86% similarity with SARS-CoV. SARS-CoV-2 shares a high degree of homology to SARS-like coronaviruses isolated in bats, suggesting that bats are the probable origin of both SARS-CoV and SARS-CoV-2.
SARS-CoV-2 virus uses the angiotensin-converting enzyme (ACE)-2 receptor to gain entry into cells. ACE-2 is found on alveolar cells of the lung epithelium of the lower respiratory tract and is also widely expressed in the cardiovascular system, kidneys, and brain.
COVID-19 appears to be highly transmittable and is primarily transmitted from human to human via upper respiratory droplets from those infected. Viral shedding in feces has also been reported. Undiagnosed asymptomatic individuals infected with COVID-19 can act as carriers and transmit the disease.
The transmissibility of a virus is indicated by its reproductive number (R0), which represents the average number of people to which a single infected person will transmit the virus. Currently, the COVID-19 R0 is estimated to range from 2.24 to 3.58. An outbreak with a R0<1 will gradually disappear. For comparison, the R0 for the common flu is 1.3 and for SARS was 2.
The COVID-19 median incubation period is estimated at 5.1 days, with 97.5% of patients becoming symptomatic at 11.5 days after being infected.
The COVID-19 case fatality rate (CFR) is estimated to range from 0.3% to 3.4%, with CFRs as high as 11% reported. Based on the Diamond Princess cruise ship data, the CFR for ship occupants was 0.99%. Although highly transmissible, the CFR of COVID-19 is lower than that of SARS (9.5%) and MERS (34.4%), but higher than influenza (0.1%).
Symptomatic COVID-19 patients typically present with systemic and/or respiratory symptoms, which typically include fever (up to 90%), cough (up to 70%), fatigue (up to 40%), sputum production (up to 35%), shortness of breath (up to 20%), and myalgia/arthralgia (up to 15%). Approximately 6% of COVID-19 patients require ventilation support. Common reported COVID-19 complications include acute respiratory distress syndrome (most common), acute cardiac injury, secondary infection and sepsis, acute kidney injury, and multiorgan failure.
Children are affected to a lesser degree by COVID-19 compared with adults. Infected children demonstrate a milder clinical course with an incubation period that is shorter by two days.
Reverse transcription polymerase chain reaction (RT-PCR), the definitive test for COVID-19, is highly specific, but false-negative rates range from 60% to 97%. Thus, patients with COVID-19 may have lung abnormalities on CT but an initially negative RT-PCR.
Up to 50% of patients with COVID-19 infection may have a normal chest CT, especially early on, after onset of flulike symptoms (days <4). On CT imaging, the disease typically progresses from GGO to GGO with superimposed inter- and intralobular septal thickening (crazy-paving pattern) to consolidations. Bilateral focal or multifocal basal, subpleural, and peripheral GGO, consolidations, or both are the most common chest CT findings, which mimic those of atypical or organizing pneumonia. Crazy paving and consolidation become the dominant CT findings as the disease peaks on imaging between nine and 13 days after illness onset. Lung abnormalities typically resolve at one month and beyond.
The findings on chest imaging related to COVID-19 are not specific and overlap with other infections. Also, a normal chest CT does not mean a person does not have a COVID-19 infection. Therefore, the ACR recommends that CT not be used to screen for or as a first-line test to diagnose COVID-19.
Droplet-type precautions, which include a medical mask, gown, gloves, and eye protection, should be in place for COVID-19 patients. Aerosol-generating procedures require N95 masks and aprons. Patients that require transport to other departments must wear a mask. SARS-CoV-2 can exist on surfaces for up to 72 hours, reinforcing the need for protection of equipment with barriers, such as covers, and thorough cleaning of equipment between patients.
A specific antiviral therapy for COVID-19 does not currently exist. Remdesivir, a drug originally developed to treat the Ebola virus, has shown promising in vitro results against COVID-19 and is currently undergoing phase III trials. Early reports demonstrate that treatment with two antimalarial drugs, chloroquine and hydroxychloroquine, has a beneficial effect on the clinical outcome. Both drugs demonstrate anti-COVID-19 activity in vitro.
— Michelle J. Romero, MD, is a radiologist at Radiology Associates of Hartford and Saint Francis Comprehensive Women’s Health Center in Hartford, Connecticut.
— Swapnil Bagade, MD, is a radiologist at Radiology Associates of Hartford and Saint Francis Comprehensive Women’s Health Center.
— Alex Merkulov, MD, is an associate professor of radiology at UConn Health at the University of Connecticut.
Resources
1. Guan CS, Lv ZB, Yan S, et al. Imaging features of coronavirus disease 2019 (COVID-19): evaluation on thin-section CT. Acad Radiol. 2020;S1076-6332(20):30143-30144.
2. Li M, Lei P, Zeng B, et al. Coronavirus disease (COVID-19): spectrum of CT findings and temporal progression of the disease. Acad Radiol. 2020;S1076-6332(20)30144-30146.
3. Mossa-Basha M, Meltzer CC, Kim DC, Tuite MJ, Kolli KP, Tan BS. Radiology department preparedness for COVID-19: radiology scientific expert panel [published online March 16, 2020]. Radiology. doi: 10.1148/radiol.2020200988.
4. Wang Y, Dong C, Hu Y, et al. Temporal changes of CT findings in 90 patients with COVID-19 pneumonia: a longitudinal study [published online March 19, 2020]. Radiology. doi: 10.1148/radiol.2020200843.
5. Wilder-Smith A, Chiew CJ, Lee VJ. Can we contain the COVID-19 outbreak with the same measures as for SARS? [published online March 5, 2020]. Lancet Infect Dis. doi: 10.1016/S1473-3099(20)30129-8.
6. Ye Z, Zhang Y, Wang Y, Huang Z, Song B. Chest CT manifestations of new coronavirus disease 2019 (COVID-19): a pictorial review [published online March 19, 2020]. Eur Radiol. doi: 10.1007/s00330-020-06801-0.

