 On the Case
On the Case
By Anna Luisa Kuhn, MD, PhD; Jasmeet Singh, MD; and Ajit S. Puri, MD
Radiology Today
Vol. 23 No. 3 P. 30
History
A 67-year-old man presented to our clinic with progressive burning and aching ranging from the sternum down to both knees. The patient underwent an imaging workup with MRI and a spinal angiogram.
Findings
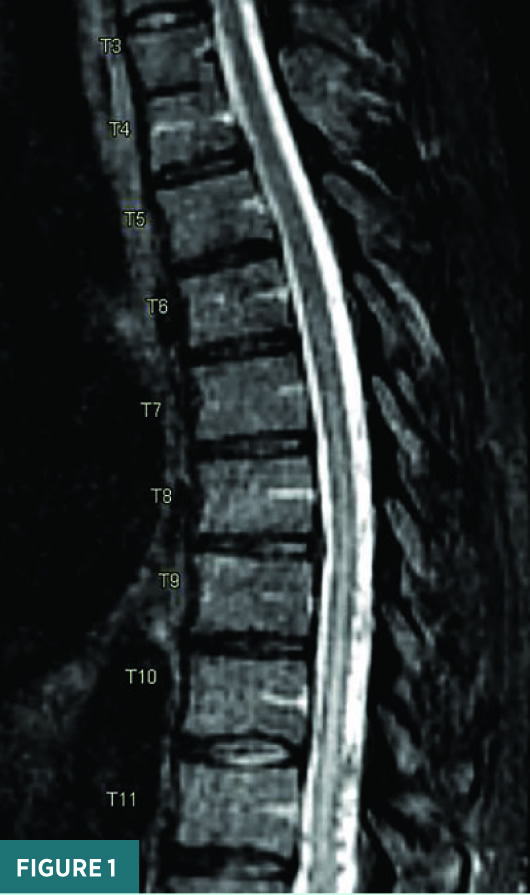
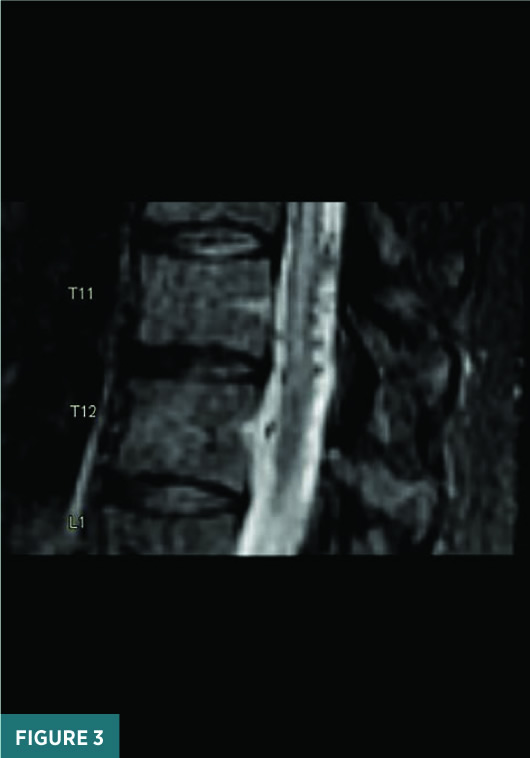
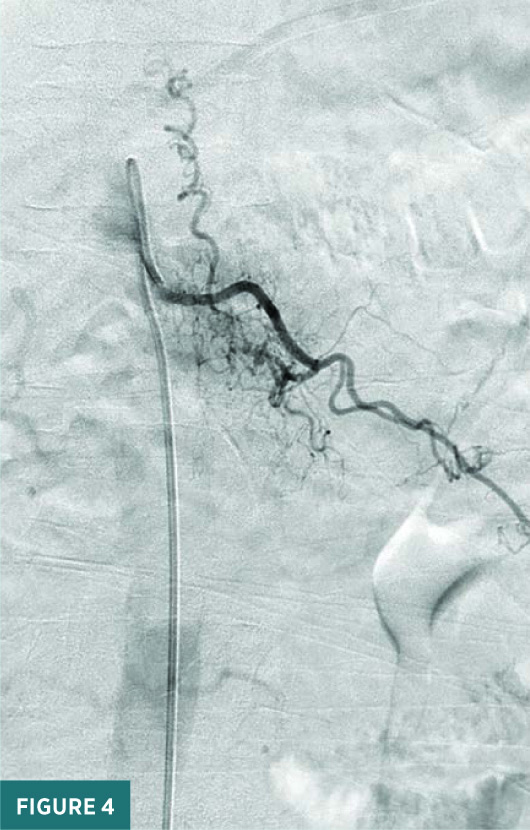
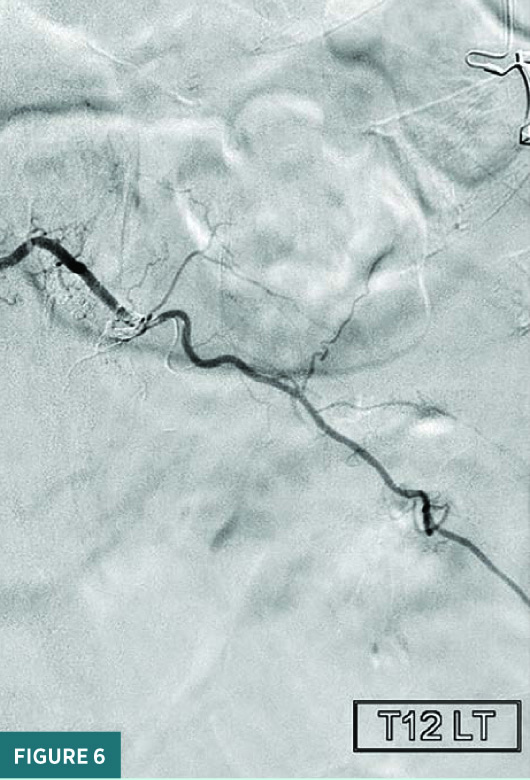
Noncontrast sagittal short tau inversion recovery (STIR) and axial T2 MRI images of the thoracic spine demonstrated a long segment of central cord signal hyperintensity (Figures 1 and 2). A magnified sagittal STIR MRI image at the T11/T12 level raised the suspicion for flow voids on the surface of the cord (Figure 3). A frontal view spinal angiogram revealed a dural arteriovenous fistula arising from the left T12 segmental artery. A selective T12 segmental artery angiogram via microcatheter contrast injection further delineated the vascular anatomy of the dural arteriovenous fistula with clear identification of the fistulous connection between the vein and the artery (Figure 4). A frontal intraprocedural radiograph shows the Onyx cast after successful embolization of the dural arteriovenous malformation with obliteration of the fistulous connection (Figure 5). A follow-up frontal view spinal angiogram of the T12 segmental artery demonstrated no residual filling of the spinal dural arteriovenous fistula (Figure 6).


Diagnosis
Spinal dural arteriovenous fistula (SDAVF).
Discussion
SDAVFs are predominant in male patients between 50 and 60 years of age. Most SDAVFs develop spontaneously; the remainder are caused by trauma.1 An SDAVF represents an abnormal connection between a medullary artery and a draining vein. The direct high-pressure arterial inflow into the vein raises the venous pressure (venous hypertension), leading to enlargement of the veins (venous congestion). With progressive failure of the draining veins, patients’ symptoms will worsen. If not appropriately diagnosed and treated, disease progression may result in irreversible cord damage.
Patients may present with progressive back pain, lower extremity weakness, and sensory changes. Given that the symptoms are mostly nonspecific, diagnosis of an SDAVF is often delayed.
Venous hypertension and congestion result in cord edema, which manifests as signal hyperintensity on MRI. Occasionally, due to enlargement of the draining veins, prominent, serpiginous flow voids are seen on the cord surface.
Digital subtraction angiography is the gold standard for diagnosis of an SDAVF and may provide options for endovascular treatment. Catheter-directed embolization of the SDAVF can be either performed with cyanoacrylate glue or Onyx. Surgical treatment consists of a targeted laminectomy with disconnection and coagulation of the draining vein.2
— Anna Luisa Kuhn, MD, PhD, is an assistant professor in the division of neurointerventional radiology in the department of radiology at the University of Massachusetts Medical Center in Worcester, Massachusetts.
— Jasmeet Singh, MD, is an associate professor in the division of neurointerventional radiology in the department of radiology at the University of Massachusetts Medical Center.
— Ajit S. Puri, MD, is a professor in the division of neurointerventional radiology in the department of radiology at the University of Massachusetts Medical Center.
References
1. Osborn AG. Diagnostic Neuroradiology. Maryland Heights, MO: Mosby Inc; 1994.
2. Morris JM. Imaging of dural arteriovenous fistula. Radiol Clin North Am. 2012;50(4):823-839.

