 Billing and Coding: A View From Health Care’s Leading Edge — 3D Printing, Elastography, and More
Billing and Coding: A View From Health Care’s Leading Edge — 3D Printing, Elastography, and More
By Melody W. Mulaik, MSHS, CRA, FAHRA, RCC, CPC, CPC-H
Radiology Today
Vol. 20 No. 8 P. 8
Radiology is a dynamic specialty that arguably leads the health care industry in the advancement of new technologies. Think of imaging today as compared with 20 years ago. Very few specialties can boast the volume of new equipment and new procedures that have been introduced in such a short period of time.
One of the challenges often associated with offering new services and/or integrating new equipment and technologies is justifying the cost or offsetting the loss of revenue associated with a nonreimbursed procedure. Although a new procedure may be widely accepted in the medical community as safe and effective for the detection and/or treatment of a disease or illness, that is no guarantee that Medicare, or any other third-party payer, will provide payment for it. Thus, organizations that provide state-of-the-art procedures are often considered to be on the “bleeding edge” of health care; they are providing a valued clinical service with little or no standard reimbursement for their efforts. This article will highlight a few new leading-edge services to ensure that your organization is appropriately assigning procedure codes.
The types of procedures that fit into this category generally have one of three options for coding assignment and submission. For the first two options, there is either a Category 1 or 3 CPT procedure code that the payers choose not to reimburse. Category 1 codes are considered the “regular” five-digit procedure codes. Category 3 codes have four numerical digits plus the letter “T” at the end, eg, 0508T.
The third option applies when a procedure must be assigned an “unlisted” CPT code because there is not a code that accurately describes the service. Per CPT Manual, “Do not select a CPT code that merely approximates the service provided. If no such procedure or service exists, then report the service using the appropriate unlisted procedure or service code.” A great example of a procedure that started as an unlisted code but graduated to a regular code with reimbursement is breast tomosynthesis. This onetime leading-edge, bleeding-edge technology has become an industry standard, with Medicare leading the way to provide coverage. Examples of procedures that meet this exception today include 3D printing, computer-aided detection for breast ultrasound, ultrasound specimen imaging, and prostate ultrasound with MRI image fusion. Not all procedures that require the use of an unlisted code would be considered a leading-edge procedure, but most do fall into this category. Let’s examine some scenarios that fit into each of these categories.
Ultrasound Elastography
Many times, procedure codes for new technologies start as Category 3 codes and then graduate into Category 1 codes, either through a code number change or a more extensive change involving the description(s). Elastography is a good example of this scenario.
Prior to 2019, ultrasound elastography was a Category 3 add-on code (+0346T) that was to be appended to a regular anatomical ultrasound code. Even though the coding has changed in 2019, this does not automatically mean that every payer will provide coverage for this exam.
Elastography is a technique for evaluating tissue elasticity (mechanical stiffness). It is used to identify malignant tumors, which are less elastic than nonmalignant tumors, as well as diagnose conditions (eg, fibrosis and cirrhosis) that cause an organ to increase in firmness.
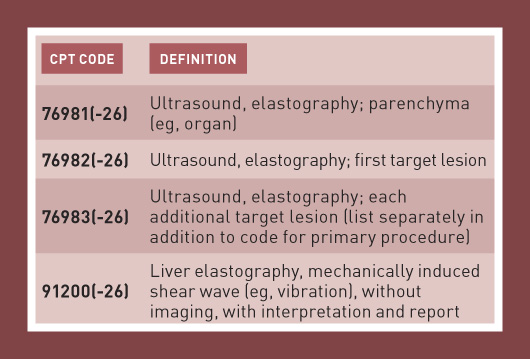
Code 76981 can be assigned only once per session per evaluation of the same parenchymal organ. If both a parenchymal organ and lesion(s) in the same organ are evaluated in the same session, assign code 76981 only. Add-on code 76983 is only reported with code 76982 and cannot be reported more than two times per organ.
Code 91200 represents nonimaging liver elastography. This includes mechanical shear wave liver elastography—also known as transient elastography—as well as acoustic radiation force impulse liver elastography—see CPT Assistant, October 2017. An example of 91200 is the FibroScan, which produces a numeric value, not an image. Note that code 91200 is restricted to exams of the liver.
Either imaging elastography (76981¬–76983) or nonimaging elastography (91200) can be performed in conjunction with diagnostic ultrasound of the liver (76700–76705). The National Correct Coding Initiative edits bundle the abdominal ultrasound into 91200, and it is appropriate to apply modifier 59 to the ultrasound code to show that it represents a separate service—see the ACR Radiology Coding Source, January/February 2015, and Clinical Examples in Radiology, Spring 2015. However, it is inappropriate to report 91200 together with an ultrasound code when an imaging elastography exam was performed. In that case, the appropriate elastography code, rather than 91200, must be assigned. So you can see that, even though there are codes, great care must be taken to ensure that they are assigned appropriately and accurately to reflect the performed services.
Sacroplasty
Sacroplasty is a procedure that has been performed for many years but is still represented by Category 3 CPT codes (0200T–0201T). Sacroplasty is vertebral augmentation of the sacrum, performed to treat osteoporotic sacral fractures.
The most common type of fracture is a vertical crack that appears alongside the sacroiliac joint on one or both sides. The physician creates a cavity by inflating a balloon, inserting an implant, or using instruments to remove some of the bone, and then cement is injected into the cavity through a needle under fluoroscopy or CT guidance. Cement injection without cavity creation should be coded as sacral vertebroplasty (22511), not sacroplasty—the January 2015 issue of CPT Assistant incorrectly stated that cement injection without cavity creation could be coded as sacroplasty, but a correction was published in the April 2015 issue.
Bone biopsy is included when performed at the same level as the sacroplasty—see CPT Assistant, December 2015. Biopsy of other vertebrae can be coded separately. The sacroplasty codes are contractor priced, so each Medicare contractor can determine whether to cover them and, if covered, how much to reimburse. Some payers do not cover sacroplasty because they consider it to be investigational.
3D Printing
A 3D printer can create a 3D object by depositing layers of material in response to a computer program. These devices are growing in popularity in the medical field, as they give health care professionals the ability to generate a model of an organ or other body structure for use in surgical planning or education.
Radiology groups and imaging centers that have 3D printers may be asked to create these models for treating physicians. However, if the provider performs 3D postprocessing of a CT or MR data set in order to create the model, the postprocessing can be reported with the 3D rendering codes (76376–76377). Keep in mind that 3D rendering cannot be reported for postprocessing of a CT angiograpy or MR angiography data set—see Clinical Examples in Radiology, Winter 2017, Summer 2018.
Effective July 1, the American Medical Association has approved Category 3 CPT codes 0559T and 0560T, which are geared toward reimbursement for the production of individually prepared 3D-printed anatomical models that can be made up of one or more components with unique colors and materials, and 0561T and 0562T, which cover the production of personalized 3D-printed anatomic guides using patient imaging data. The new codes do not guarantee payment, however.
Whole-Body Scans
The performance of whole-body scans for cancer detection have resurfaced in the coding discussion for both CT and MRI. For example, the National Comprehensive Cancer Network has included a whole-body MRI scan as an option to detect multiple myeloma. According to Clinical Examples in Radiology, Spring 2009, a “whole-body MRI should be reported with the unlisted MRI code 76498.”
Similarly, there is not a specific CPT code to describe the whole-body CT scan for diagnosis or screening. According to Clinical Examples in Radiology, Summer 2018, “When performed and medically necessary, code 76497, Unlisted computed tomography procedure (eg, diagnostic, interventional), is reported. If only certain anatomical areas are identified for CT evaluation, those anatomical regions should be coded accordingly.”
Other Unlisted Procedures
In the absence of policies that specifically address a procedure, unlisted codes require a detailed report from the physician including the complexity of the medical condition, any physical findings, and the extent of the procedure, including time, skill, and any specialized equipment necessary to provide the service. All insurance payers monitor and manually review claims filed with “unlisted” procedure codes. It is recommended that the elements of a detailed report include the following:
• a detailed description of the procedure performed;
• copies of articles in medical journals, etc, providing clinical trial information, medical indications, patient outcomes, and surgery or other procedure replaced by the new procedure;
• documentation of the medical necessity of the procedure;
• time, effort, and equipment required to perform the procedure;
• any cost savings experienced by utilizing this procedure;
• patient diagnosis, chief complaint, and presenting symptoms and signs;
• any concurrent problems requiring treatment or management;
• description of follow-up care and prognosis;
• relation of the “unlisted” procedure to an existing procedure in terms of the amount of physician work involved or facility resources expended; and
• financial quantification of cost savings to the payer when more extensive procedures are avoided, if applicable.
Including all of the recommended information may seem like a daunting task; however, it may be the worth the effort if your facility is frequently performing leading-edge procedures.
Radiology will continue to be at the forefront of medicine, but, unfortunately, reimbursement will generally lag behind. Make sure all of your financial analyses that incorporate reimbursement are realistic, accurate, and in accordance with correct coding guidelines. Also ensure that you are always up to date on the latest coding guidelines—remember, the only constant is change!
— Melody W. Mulaik, MSHS, CRA, FAHRA, RCC, CPC, CPC-H, is the president of Coding Strategies, Inc & Revenue Cycle, Inc.

