 On the Case
On the Case
By Elena G. Violari, MD, and Alex Merkulov, MD
Radiology Today
Vol. 18 No. 9 P. 25
History
A 73-year-old woman with a history of depression presented to the emergency department (ED) with vague abdominal pain for the third time in two weeks. There was no hematemesis, hematochezia, or melena. During prior ED visits, she underwent two noncontrast CT examinations of the abdomen and pelvis, neither of which revealed a clinically significant abnormality. On her third ED visit, an IV contrast-enhanced CT of the abdomen and pelvis was performed.
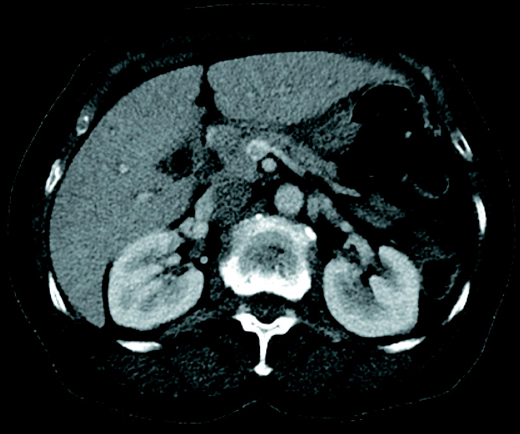
An axial contrast-enhanced CT image showed a filling defect within the superior mesenteric vein (SMV) [Figure 1]. Sagittal and coronal reformatted multidetector CT images depicted thrombotic extension involving the SMV [Figures 2 and 3].


Diagnosis
SMV thrombosis (SMVT).
Discussion
The patient was admitted to the hospital for disease management and pain control. On admission, she was afebrile and did not have an elevated white blood cell count. She did have mildly elevated alanine transaminase (63) and alkaline phosphatase (161). There was no CT evidence of small bowel wall thickening, mesenteric fat stranding, or ascites to suggest bowel ischemia. The patient was placed on Lovenox and started on Coumadin. She was eventually started on a clear diet and advanced to a full diet. She was discharged home on Lovenox injections as a bridge to Coumadin.
The SMV drains blood from the jejunum and ileum. At its termination behind the neck of the pancreas, the SMV combines with the splenic vein to form the hepatic portal vein.
SMVT is rare and can cause a variety of symptoms, including progressively worsening, diffuse, colicky abdominal pain; anorexia; abdominal distention; and heme-positive stool. It is not uncommon for symptoms to have been present for several days.
SMVT is recognized to occur in acute, subacute, and chronic subtypes. Acute SMVT, defined as new-onset symptomatic thrombosis of the SMV or its branches without evidence of collateralization, typically presents with abdominal pain and, similar to arterial types of acute mesenteric ischemia, may lead to intestinal infarction unless diagnosed and treated promptly. Subacute and chronic SMVT may be asymptomatic due to venous collateralization and are unlikely to cause intestinal infarction.
Hypercoagulable states secondary to malignancy, polycythemia vera, protein C or S deficiency, recent abdominal surgery, sepsis, portal hypertension, or mechanical narrowing are the most common predisposing factors to mesenteric venous thrombosis. Twenty percent to 40% of cases are considered idiopathic, as they do not have a clear precipitating factor.
Because the symptoms of mesenteric venous thrombosis are nonspecific, imaging is the best and most reliable way of making the diagnosis. CT is an established noninvasive technique for the visualization of the intestinal vasculature with excellent sensitivity (up to 100%). Ultrasound and catheter mesenteric angiography reportedly have approximately 70% sensitivity but are infrequently requested as a first-line investigation, unless the presentation (eg, cholecystitis) suggests another diagnosis.
Management of mesenteric vein thrombosis includes both operative and nonoperative approaches. Operative interventions include thrombectomy with thrombolysis; this is often employed for patients who present with signs of peritoneal irritation. Patients with intestinal infarction must undergo surgical resection of the infarcted bowel segment, followed by anticoagulation. Approximately 14% of those who undergo bowel resection will, usually within six weeks, have a repeated mesenteric vein thrombosis.
Anticoagulation is an efficacious treatment option for patients with mild symptoms or with subacute/chronic SMVT. Endovascular thrombolysis/thrombectomy is another viable option in patients without intestinal infarction.
— Elena G. Violari, MD, is a radiology resident at UConn Health at the University of Connecticut.
— Alex Merkulov, MD, is an associate professor of radiology at UConn Health at the University of Connecticut.
Resources
1. Gaspary MJ, Auten J, Durkovich D, Gable P. Superior mesenteric vein thrombosis mimicking acute appendicitis. West J Emerg Med. 2011;12(2):262-265.
2. Hmoud B, Singal AK, Kamath PS. Mesenteric venous thrombosis. J Clin Exp Hepatol. 2014;4(3):257-263.
3. Klar E, Rahmanian PB, Bücker A, Hauenstein K, Jauch KW, Luther B. Acute mesenteric ischemia: a vascular emergency. Dtsch Arztebl Int. 2012;109(14):249-256.
4. Walker TG. Mesenteric ischemia. Semin Intervent Radiol. 2009;26(3):175-183.

