 On the Case
On the Case
By Michael A. Simon, MD; Tate B. Hodges, MD; Julia S. Gesner; Ning Lu, MD; Lyle Gesner, MD; and Rahul V. Pawar, MD
Radiology Today
Vol. 22 No. 7 P. 30
History
A 76-year-old man presented to the emergency department (ED) and reported difficulty walking. One week prior to admission, the patient had fevers and myalgias, which resolved with over-the-counter medication. Since that time, the patient noted progressive lower extremity weakness leading to his presentation to the ED. Physical examination was significant for two-fifths strength in the bilateral lower extremities. Plantar flexion and dorsiflexion were also reduced bilaterally. No rashes or skin abnormalities were noted. Amid concern for Guillain-Barre syndrome (GBS), MRI of the lumbar spine with contrast was performed.
Findings
MRI of the lumbar spine with (Figures 1 and 2) and without (Figures 3 and 4) IV contrast demonstrated avid enhancement of the cauda equina, particularly of the ventral nerve roots. The enhancement pattern was suggestive of an inflammatory demyelinating polyradiculopathy process such as GBS.
The patient subsequently underwent a lumbar puncture, which was significant for cerebrospinal fluid pleocytosis and varicella zoster DNA. The patient was started on IV acyclovir and stress dose steroids with rapid improvement of his symptoms.
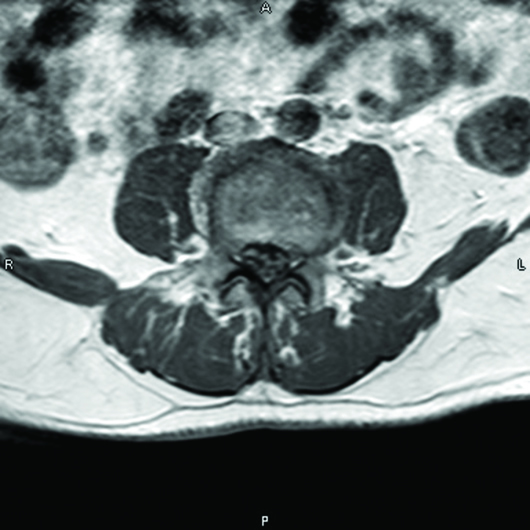
Figure 1

Figure 2
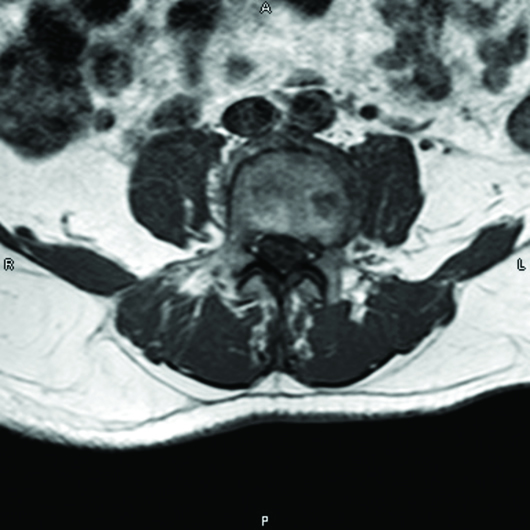
Figure 3

Figure 4
Diagnosis
Zoster sine herpete (ZSH).
Discussion
Primary infection with the varicella zoster virus (VZV) leads to development of a rash, commonly referred to as “chicken pox.” Following primary infection with VZV, the virus can remain dormant in the cranial nerves, dorsal root, and/or autonomic ganglion.1 Under a variety of conditions, VZV can reactivate, causing herpes zoster, the hallmark of which is a painful cutaneous vesicular rash in a dermatomal distribution.2 This disease is common in the United States, with an incidence of 7.2 in 1,000 cases of VZV.3
Herpes zoster can cause multiple various neurological and ocular disorders including myelopathy, Ramsay Hunt syndrome, and herpes zoster ophthalmicus. Neurologic symptoms outside the rash dermatome are rare and termed ZSH.
ZSH was first described by Widal in 1907 in a patient with thoracic pain and hyperesthesia, in a region outside of the dermatomal vesicular rash.4 In 1916, Weber described two patients with segmental pain in a dermatomal distribution who subsequently developed facial and truncal zoster.5 Lewis described a cohort of 120 patients who experienced pain in a dermatomal distribution outside the rash dermatome.6 Additional case reports have described the various manifestations of ZSH, including the presence of neuropathic pain in a dermatomal distribution, paresis, ophthalmic neuralgia, otalgia, and abdominal pain.1,7 To our knowledge, no case reports were found that describe the presence of isolated symptoms of cauda equina syndrome in a patient with VZV reactivation.
As these symptoms are not associated with a rash, diagnosis can be difficult. To further confound matters, the presence of isolated symptoms of cauda equina syndrome, specifically progressive lower extremity weakness, can easily be associated with GBS. As treatment of these two disease processes differ—GBS is treated with IV immune globulin and herpes zoster is treated with IV acyclovir—it is imperative to perform additional testing with lumbar puncture to ensure proper treatment. The cerebrospinal fluid in a patient with GBS typically is significant for elevated protein levels without pleocytosis. The opposite is expected in a patient with herpes zoster infection, where pleocytosis, elevated protein, and the presence of VZV DNA is expected. These differences allow for a clear final diagnosis and appropriate treatment.2
In conclusion, it is important to keep ZSH in the differential for patients with regional pain and/or neurological symptoms with a history of prior infection with VZV. This will allow for timely treatment and prevention of severe sequela of the disease.
— Michael A. Simon, MD, is a radiology resident at Saint Barnabas Medical Center in Livingston, New Jersey.
— Tate B. Hodges, MD, is a radiology resident at Saint Barnabas Medical Center.
— Julia S. Gesner is a student at Lafayette College in Easton, Pennsylvania.
— Ning Lu, MD, is a radiologist at Saint Barnabas Medical Center.
— Lyle Gesner, MD, is a radiologist at Saint Barnabas Medical Center.
— Rahul V. Pawar, MD, is a radiologist at Saint Barnabas Medical Center.
References
1. Kennedy PGE. Zoster sine herpete: it would be rash to ignore it. Neurology. 2011;76(5):416-417.
2. Zhou J, Li J, Ma L, Cao S. Zoster sine herpete: a review. Korean J Pain. 2020;33(3):208-215.
3. Steinberg CJ, Moody AD, Yenior AL, Bertasi RAO, Kieneker L, Pujalte GGA. Disseminated herpes zoster with cauda equina symptoms. IDCases. 2020;21:e00902.
4. Widal G. Le Zona fruste. J Med Chir Prat. 1907;78:12-14.
5. Weber FP. Herpes zoster: its occasional association with a generalized eruption and its occasional connection with muscular paralysis. Int Clin. 1916;3:185-202.
6. Lewis GW. Zoster sine herpete. Br Med J. 1958;2(5093):418-421.
7. Edelman DA, Antaki F, Basson MD, Salwen WA, Gruber SA, Losanoff JE. Ogilvie syndrome and herpes zoster: case report and review of the literature. J Emerg Med. 2010;39(5):696-700.

