November 30, 2009
Risk Management & Malpractice Defense
Pitfalls of the Vague Radiology Report
By Leonard Berlin, MD, FACR
Radiology Today
Vol. 10 No. 19 P. 10
Editor’s Note: Leonard Berlin, MD, FACR, is a professor of radiology at Rush University Medical College and the chairman of the department of radiology at Rush North Shore Medical Center in Skokie, Ill. He began writing on risk management and malpractice issues in a series of articles in the American Journal of Roentgenology. Those articles became the basis for his well-known book Malpractice Issues in Radiology. The third edition is available from the American Roentgen Ray Society (www.arrs.org).
Vague: wandering, roaming, unsettled, uncertain … not definite in meaning, not explicit or precise, of indistinct ideas … absence of clear perception or understanding … meaningless.1
The Cases
Case 1.
A 37-year-old man underwent routine chest radiography (Fig. 1A) that was interpreted by the radiologist as:
A 1 X 1.5 cm nodular density is projected over the anterior portion of the right second rib in the right suprahilar region. It is not clear whether this is due to overlapping shadows, an area of increased density within the rib, or a pulmonary nodule. Appearance suggests a granuloma. Nevertheless, a follow-up chest film in 3 to 4 months is recommended to evaluate this finding.
Chest radiography obtained 3 months later (Fig. 1B) was interpreted by the same radiologist as:
There is a persistent nodular density in the right suprahilar region, unchanged since previous study. Although I suspect this is due to overlapping vascular shadows, correlation with computed tomography of the region may be of value to definitely exclude a pulmonary nodule.
No follow-up chest radiography or CT was performed until 1 year later, at which time a large right-lung tumor was easily seen (Fig. 1C). Biopsy disclosed adenocarcinoma.
Case 2.
A 42-year-old man who had been treated in the past for a soft-tissue sarcoma of the left lower extremity underwent chest radiography (Figs. 2A and 2B). The radiologist rendered the following interpretation:
There is a 4 cm density in the frontal projection on the left, which in the lateral view appears to lie in the major fissure and is compatible with a pseudotumor. Comparison with the patient’s prior films is recommended to assess whether this represents an acute or chronic finding. The chest is otherwise unremarkable.
No follow-up radiologic studies were performed until 6 months later, at which time chest radiographs revealed a large round 12-cm-diameter mass in the left lung (Figs. 2C and 2D). Biopsy disclosed recurrent sarcoma.
Case 3.
Chest and abdominal radiography was performed on a 61-year-old woman because of abdominal pain (Fig. 3A). The study was interpreted by the radiologist as follows: “Normal abdominal and chest radiographs except for band of atelectasis or infiltrate in the left lung base.”
Although the abdominal pain subsided spontaneously, follow-up chest radiography was performed 1 week later (Fig. 3B). The radiographic findings were “small patchy increased density in left lung base that is stable and probably chronic.”
Follow-up chest radiographic findings obtained 7 weeks later (Fig. 3C) were reported by the radiologist simply as “slight decrease in left lung base density.”
Ten months later, the patient was seen by physicians at another facility. There, radiographs disclosed a well-defined 3-cm tumor in the left lower lobe. Biopsy revealed carcinoma.
Case 4.
A 53-year-old man underwent chest radiography as part of a preemployment physical examination (Fig. 4A). The radiologist interpreted the study as follows: “Normal except for an ill-defined density present in the right upper lobe that is probably an artifact, but if indicated, a repeat view is suggested.”
The patient did not return for follow-up studies until 2 years later. At that time, chest radiography disclosed a tumor in the right upper lobe (Fig. 4B). Biopsy confirmed squamous cell carcinoma.
Case 5.
A 59-year-old woman underwent an upper gastrointestinal radiography because of dysphagia and epigastric fullness (Fig. 5). The radiologist issued the following report: “Irregularity in the cardia of the stomach. Small hiatal hernia.”
No additional diagnostic studies were obtained at the time. Ten months later, the patient underwent endoscopic examination that revealed a large lesion of the cardiac portion of the stomach. Biopsy confirmed the presence of adenocarcinoma.
Case 6.
A 55-year-old man with epigastric discomfort underwent upper gastrointestinal radiography (Fig. 6). The radiologist interpreted the study as follows:
There is gastroesophageal reflux and irregularity of the distal esophageal mucosa compatible with peptic esophagitis and a possible stricture. Reexamination of the esophagus after appropriate medical therapy with either endoscopy or esophagram is recommended.
The patient did not return to his physician until 14 months later. Endoscopy and biopsy at that time revealed carcinoma of the esophagus.
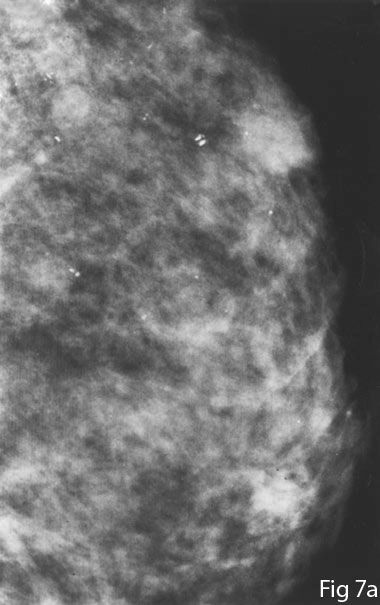
Case 7.
A 57-year-old woman underwent screening mammography (Fig. 7A). The radiologist interpreted the mammograms as follows:
There is an asymmetrical area of increased density and prominent dysplasia with benign-appearing calcifications in the upper outer quadrant of the right breast. Clinical correlation and follow-up studies are recommended to exclude a mass.
Eight months later, the patient consulted her physician because of a palpable lump in the breast. Mammography now revealed two masses highly suggestive of malignancy (Fig. 7B). Biopsy disclosed invasive ductal carcinoma.
Malpractice Issues
In the seven cases described, attorneys representing the patients in whom the diagnosis of cancer was delayed filed medical malpractice lawsuits against the interpreting radiologists.
Cases 1-4. The four cases alleging delay in diagnosis of lung cancer resulted in the filing of malpractice lawsuits, all of which were settled before trial. Payments made on behalf of the defendant radiologists were not disclosed in cases 1,2, and 3. In case 4, a settlement of $1 million was agreed to on behalf of the defendant radiologist and codefendant.2
Cases 5-7. Large settlements were paid on behalf of the defendant radiologists in cases 5 and 6, in which lawsuits alleging delay in diagnosis of gastrointestinal malignancies had been filed. Case 5 was settled for a total of $900,0003 and case 6 was settled for $1.25 million. The malpractice lawsuit in case 7, dealing with an alleged delay in diagnosis of breast cancer, was settled with a payment of $1.5 million on behalf of the defendant radiologist.
Discussion
The common thread that binds these seven cases is the nature of the radiology reports—or to be more specific, the vagueness of the radiology reports. The reports were not truly inaccurate—the chest radiographs in cases 1, 2, and 4 did reveal abnormal densities that were not obviously indicative of malignancies; the radiographs in case 3 did disclose nonspecific left lower lobe infiltration; the findings in the distal esophagus and proximal stomach in cases 5 and 6 were described with reasonable objectivity; and an asymmetric density was present on the mammogram in case 7. Notwithstanding the likelihood that most radiologists might judge these radiology reports as reasonably accurate in every one of these cases, the referring physicians failed to take action that would have led to the prompt diagnosis of malignancy. We must, therefore, ask ourselves who, if anyone, was at fault and why.
The delay in diagnoses and the ensuing medical malpractice litigation that took place in these cases may well have been the result of simple carelessness and lack of follow-up on the part of the referring physicians. On the other hand, we cannot ignore the possibility that these events also could have been the result of inadequate if not negligent reporting on the part of the interpreting radiologists. We know what the attorneys and insurance companies that agreed to settle the eight cases thought: They determined that both the referring physicians and the interpreting radiologists were negligent and, therefore, jointly liable for injuries sustained by the patients. The legal culpability attributed to the radiologists clearly stems from a problem with a key link of the information chain that connects radiologists to their referring physicians—namely, the radiology report. Let us now further analyze that key link—the radiology report.
Over the years, a number of commentators in the radiology literature have discussed the subject of radiology reports. Three quarters of a century ago, Enfield4 criticized radiologists who issued written radiology reports that
…describe in detail all that the roentgenologist sees in the film or on the screen but does not tell what he thinks about it, what conclusions he draws from it, and what it means to him.
This kind of report “commits the roentgenologist to nothing except accurate vision and good description. ... It tells much, yet almost nothing,” wrote Enfield, who then exhorted radiologists to “give not only their opinion but also their method of arriving at that opinion.”
Commenting 60 years later on radiology reports, Friedman5 held that “it is the obligation of the radiologist to state what has been found as clearly and pointedly as possible.” Fischer6 added that the radiology report must be not only accurate but also meaningful. Indeed, clarity and meaningfulness were the most valued qualities of radiology reports among 200 referring physicians, according to a Canadian survey.7 Let us digress and focus on the definitions of these terms in more detail.
“Meaningful” is defined as “capable of being understood or interpreted … the thing one intends to convey by language … exhibiting a specified intent or purpose…”1 Meaningful is an antonym of meaningless, which is defined as “having no assigned function … having no significance … vague.”1 The definition of “vague” is given at the beginning of this article.
Spira8 has urged radiologists to render more meaningful reports of radiologic studies, going so far as to write that radiologists do themselves, their patients, and referring physicians a disservice when they create a vague report. He asserts:
A rambling description of findings without a reasonable conclusion does not add anything positive and often is perceived as an attempt to distance the interpreter from the clinical issue at hand … leaving the reader confused.
In its “Standard for Communication: Diagnostic Radiology,” the American College of Radiology steers away from using such words as “vague” or “meaningful” and instead states simply that the radiology report “should use precise anatomic and radiologic terminology to describe the findings accurately” and that an impression should include “a precise diagnosis … whenever possible.” The standard also mandates radiologists to “recommend follow-up or additional diagnostic studies to clarify and confirm the impression … when appropriate.”
Let us now turn to the practical and legal question that is the crux of this article: Did the seven radiology reports convey to the referring physicians a truly accurate representation of the radiologic findings, the radiologists’ opinions of the meaning of the findings, and the radiologists’ recommendations for further action to the referring physicians?
In each of the cases described, the referring physicians testified either in deposition or at trial or stated off the record to their attorneys that if the radiologists had only been stronger in their reports, they would have acted (to pursue a diagnosis) much sooner. In some of the cases, the defendant radiologists acknowledged that the complaints of the referring physicians had merit; but in other cases, the radiologists did not agree with the complaints.
Communication between two individuals is, of course, a two-way street. In the context of radiology reporting, sometimes the radiologist’s meaning is not accurately conveyed to the referring physician, and at other times, the referring physician misunderstands the radiologist. A failure of communication between two physician professionals is more likely because of some degree of fault in both. In not one of the seven cases discussed here did the interpreting radiologists use in their reports such phrases as “the radiographic findings are suggestive for carcinoma” or “carcinoma is possible” or “carcinoma should be considered,” all of which are meaningful phrases. In not one of the cases did the interpreting radiologist clearly recommend an additional radiologic study or biopsy, again, meaningful phrases. Such terms as “if clinically warranted” or “if clinically indicated may be of value” or “comparison with patient’s prior films is recommended” or “would be most helpful” or “may be of benefit” or “clinical correlation is recommended” were all used quite freely—but these phrases are vague rather than meaningful.
Is it because of the vagueness of these reports that the referring physicians did not obtain additional studies to diagnose carcinoma earlier? Did the language used in the radiology reports lull the referring physicians into inaction and lethargy (conduct referred to as “soporific” by Goldsmith9), rather than alert them to the fact that prompt action must be taken? Considering the amount of indemnification paid on behalf of the defendant radiologists in these cases, the answers to these questions appear to be “yes.” Although it may be true, at least in some of the cases, that the delays in diagnoses were more the result of lackadaisical if not substandard conduct of the referring physicians, the fact remains that the law holds radiologists responsible for lapses in their own conduct, irrespective of any liability that might be imposed on other physicians (Reed v Weber, Ohio, 1992). This fact should provide a wake-up call for all radiologists to review their technique of reporting.
Recognizing the wide variation and lack of uniformity of reports rendered by radiologists, Hickey10 proposed more than 80 years ago that national radiology organizations try to achieve uniform reporting by developing standardized nomenclature and writing style. Although such a system has yet to be implemented for general diagnostic radiology, it has already been accomplished in the subspecialty of mammography. The American College of Radiology instituted the Breast Imaging Reporting and Data System (BI-RADS), which consists of a lexicon of terminology and definitions to provide standardized language in reporting mammography. By providing clear and succinct language for reports, BI-RADS has achieved its goal of making communication of mammographic findings more accurate and decisive. Ambiguity and vagueness have, for the most part, been eliminated in mammography.11
Summary and Risk Management
Written interpretations by radiologists of radiologic studies are extremely important from both medical and legal perspectives. These reports provide an integral part of the medical record and are an essential link between the diagnosis and the treatment of a patient’s illness. The legal authority and importance of radiology reports were emphasized by a federal appeals court that characterized them not simply as “reports of diagnosis or opinions” but rather as “factual reports of analysis of [a patient’s] body” (Lambert v Goodyear Tire and Rubber, Ohio, 1992). The court added, “A radiologist’s enumeration of the contents of an x-ray is not … mere medical hypothesis, but, rather, a learned statement of an observable condition.”
Radiologists owe patients the interpretation of radiologic studies in a manner that is meaningful to the referring physician.12 Once a malpractice lawsuit is filed, the radiology report becomes important evidence—a legal exhibit—in the courtroom. It is then determined by a court of law whether a report rendered by a defendant radiologist clearly conveyed to the referring physician the results of a given radiologic study—that is, whether the radiologist’s report conformed to or breached the radiologic standard of care. If it is determined that the phrasing of the radiology report is insufficient to meet the standard, indemnification will be paid, through either settlement negotiations or a jury verdict. Radiologists must remember that they have an independent duty to be accurate and concise, regardless of whether the actions of the referring physician are negligent (Reed v Weber).
Risk management in radiology practice can lessen the likelihood of incurring a medical malpractice lawsuit, maximize the chance for a successful defense if a suit is filed, and at the same time enhance good patient care. The following risk management pointers will help radiologists meet all three of these objectives:
• Radiologists should heed the words of Rothman13, who wrote that because radiologists are paid for using both their eyes and their brains, a complete radiology report must include both sets of evaluations. The body of the report should contain a complete description of all abnormalities—that is, everything that is seen with the eyes—but the conclusion should discuss only those findings that are important to the brain, contended Rothman. The length of the body of the report depends on the number of findings, whereas the length of the conclusion varies with the radiologist’s ability to make sense of the findings.
• Before completing a radiology report, radiologists should ask themselves, “What do I want my referring physician to conclude from my interpretation?” The interpreting radiologist should try to address in the report the following self-imposed questions: What did I see on the radiographic studies, by what do I believe the findings are caused, and what do I suggest the referring physician do next? Radiologists should not sign their reports until these questions are answered in a meaningful manner.
• Radiologists should minimize, if not eliminate altogether, the use of such phrases as “if clinically warranted” and “if clinically indicated may be of value” when assessing abnormal radiographic findings. Because radiologists are acknowledged to possess radiologic expertise derived from training and experience, they should not relinquish to nonradiology physicians the responsibility of evaluating the potential significance of a purely radiographic finding that is unexpected or unusual.
• When rendering radiology reports, radiologists should refrain from hedging, defined as the making of calculatedly noncommittal or ambiguous statements.1 Radiologists should be mindful of the following aphorism coined by one radiology educator: “Do not let the fear of being wrong rob you of the joy of being right” (Rogers LF, personal communication).
• A report need not always be brief but it can always be concise.14 Radiologists should attempt to convey important radiologic findings as briefly as possible. Good writing is succinct, accurate, clear, and unambiguous; it grabs the attention, conveys a message, and elicits a response.15
• Readers who want specific hints as to what constitutes a good radiology report should consult specific references listed at the end of this article.3,16-18 All radiologists should read the 16 tips on how to write a radiology report by Revak.19 They are as valid today as they were when they were first published.
— This article appeared in its original form in the American Journal of Roentgenology. It is reprinted here with permission of the American Roentgen Ray Society.
References
1. Webster’s Third New International Dictionary of the English Language Unabridged. Springfield, Mass.: Merriam-Webster;1993:1048,1399,2528.
2. Berlin L. Errors in judgment. Am J Roentgenol. 1996;166(6):1259-1261.
3. Berlin L. Radiology reports. Am J Roentengol. 1997;169(4):943-946.
4. Enfield CD. The scope of the roentgenologist’s report. JAMA. 1923;80(14):999-1001.
5. Friedman PJ. Radiologic reporting: structure. Am J Roentgenol. 1983;140(1):171-172.
6. Fischer HW. Better communication between the referring physician and the radiologist. (editorial) Radiology. 1983;146:845.
7. Lafortune M, Breton G, Baudouin JL. The radiological report: What is useful for the referring physician? Can Assoc Radiol J. 1988;39(2):140-143.
8. Spira R. Clinician, reveal thyself. Appl Radiol. 1996;25(11):5-13.
9. Goldsmith SJ. If clinically indicated. J Nucl Med. 1996;37(8):3A.
10. Hickey PM. Standardization of roentgen-ray reports. Am J Roentgenol. 1922;9:422-425.
11. Kopans DB. Breast Imaging, 2nd ed. Philadelphia: Lippincott-Raven:1998:762-784.
12. Weaver JW. Equal rights for all—except for doctors. (letter) Am J Roentgenol. 1998;170(5):1395.
13. Rothman M. Malpractice issues in radiology: Radiology reports. (letter) Am J Roentgenol. 1998;170(4):1108-1109.
14. Martin LFW. Opinion: Is this your report? Can Assoc Radiol J. 1982;33:255-256.
15. Ronai PM. Plural effusions. Am J Roentgenol. 1992; 159(3):564.
16. Berlin L. Communication of the urgent finding. Am J Roentgenol. 1996;166(3):513-515.
17. Berlin L. Communication of the significant but not urgent finding. Am J Roentgenol. 1997;168(2):329-331.
18. Cascade PN, Berlin L. American College of Radiology Standard for Communication. Am J Roentgenol. 1999;173(6):1439-1442.
19. Revak CS. Dictation of radiologic reports. (letter) Am J Roentgenol. 1983;141:210.
Fig. 1, Case 1: 37-year-old asymptomatic man who underwent routine chest radiography. A, Posteroanterior radiograph shows 1 X 1.5 cm density in right suprahilar region. Radiologist concluded, “It is not clear whether this is due to overlapping shadows, an area of increased density within the rib, or a pulmonary nodule ... a follow-up chest film in 3 to 4 months is recommended to evaluate this finding.” B, Radiograph obtained 3 months after A. Radiologist reported that nodular density is unchanged and that “correlation with computed tomography of the region may be of value...” C, Radiograph obtained 1 year after B reveals extensive carcinoma.
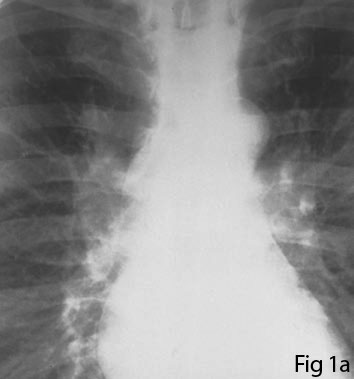

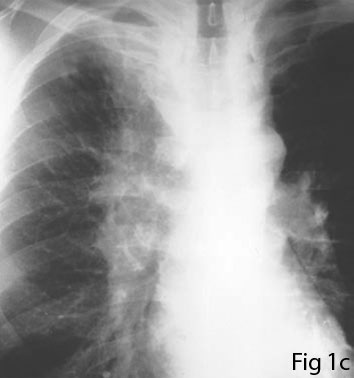
Fig. 2, Case 2: 42-year-old man who had undergone treatment for sarcoma of left extremity. A and B, Posteroanterior (A) and lateral (B) chest radiographic findings were abnormal. Radiologist reported 4-cm density on left, “which in the lateral view appears to lie in the major fissure and is compatible with a pseudotumor.” Radiologist suggested comparison with patient’s prior films. C and D, Radiographs obtained 6 months after A and B show round 12-cm diameter mass in left. Biopsy disclosed recurrent sarcoma.
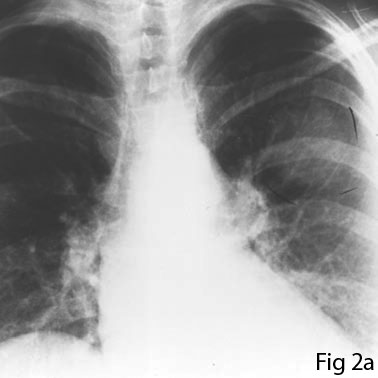


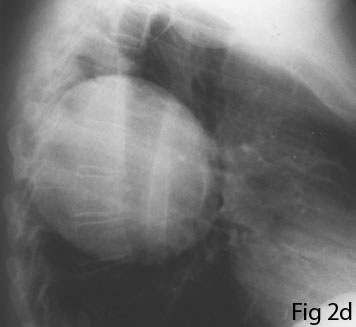
Fig. 3, Case 3: 61-year-old woman who underwent radiographic examination because of abdominal pain. A, Initial chest radiographic findings reported by radiologist were normal except for “band of atelectasis or infiltrate in the left lung base.” B, Radiograph obtained 1 week after A interpreted by radiologist as “small patchy increased density in left lung base that is stable and probably chronic.” C, Radiograph obtained 7 weeks after B, reported by radiologist as “slight decrease in left lung base density.” Ten months later, patient presented with 3-cm carcinoma in left lower lobe.

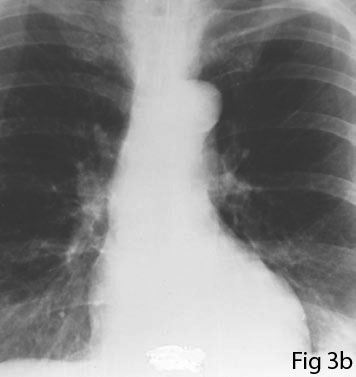
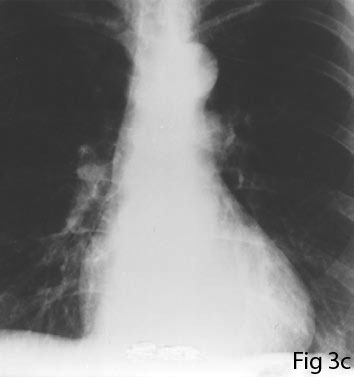
Fig. 4, Case 4: 53-year-old asymptomatic man who underwent routine chest radiography. A, On initial radiograph, radiologist reported probable right upper lobe artifact. B, Radiograph obtained 2 years after A shows large carcinoma.


Fig. 5, Case 5: 59-year-old woman who complained of dysphagia and epigastric fullness. Representative radiograph from upper gastrointestinal examination was reported by radiologist as disclosing “irregularity in the cardia of the stomach.” Ten months later, endoscopy revealed large infiltrating adenocarcinoma of cardiac portion of stomach.

Fig. 6, Case 6: 55-year-old man with epigastric discomfort who underwent upper gastrointestinal radiography. Radiologist reported study as showing “gastroesophageal reflux and irregularity of the distal esophageal mucosa compatible with peptic esophagitis and a possible stricture. Reexamination of the esopagus after appropriate medical therapy with either endoscopy or esophagram is recommended.” Fourteen months later, endoscopy revealed carcinoma of distal esophagus.
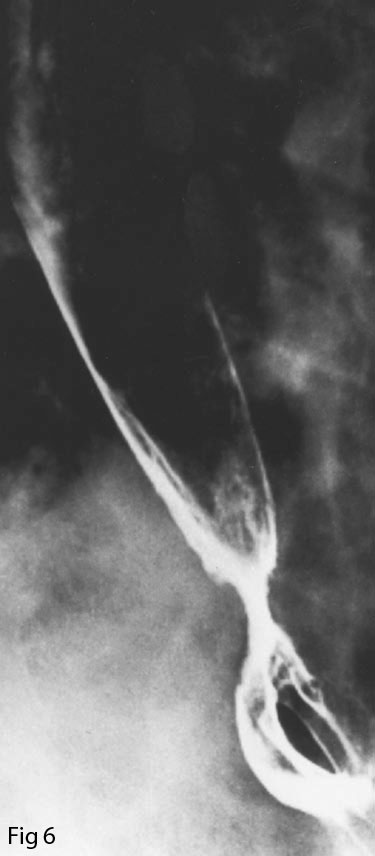
Fig. 7, Case 7: 57-year-old woman who underwent screening mammography. A, Initial mediolateral mammogram was reported by radiologist as disclosing “asymmetrical area of increased density and prominent dysplasia with benign-appearing calcifications ... Clinical correlation and follow-up are recommended...” B, Mediolateral mammogram was obtained 8 months after A because patient palpated lump. Mammography now revealed two masses suggestive of malignancy. Biopsy disclosed invasive ductal carcinoma.