 On the Case
On the Case
By Anna Luisa Kuhn, MD, PhD, and Ajit S. Puri, MD
Radiology Today
Vol. 19 No. 12 P. 30
History
A 71-year-old woman with a past medical history significant for hyperlipidemia, hypertension, coronary artery disease post myocardial infarction, a coronary artery bypass grafting procedure, a 60-pack-year history of smoking, and COPD presented for evaluation of vertigo and right arm weakness.
Findings
Cross-sectional CT imaging revealed severe atherosclerotic changes along the right innominate artery (Figures 1 and 2). A conventional diagnostic angiogram was then performed for further characterization of the stenosis and possible treatment. The left vertebral artery was the first vessel to be catheterized (Figure 3), and cervical angiography was performed. Retrograde contrast opacification of the contralateral right vertebral artery (Figure 4) and eventual contrast opacification of the right subclavian artery and the internal mammary artery was observed (Figures 5 and 6) suggesting right subclavian steal syndrome (SSS). Diagnostic angiograph evaluation of the remainder of the vessels was carried out and, eventually, a severe right innominate artery stenosis was detected. This was subsequently treated with placement of a stent. A thoracic arch aortogram depicts the postinterventional changes after successful stent placement in the right innominate artery with normal antegrade flow through the right vertebral artery (Figure 7).

Figure 1

Figure 2
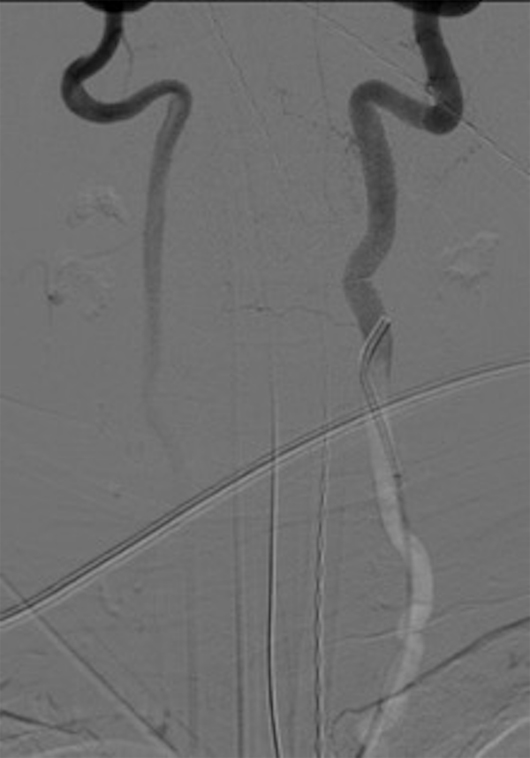
Figure 3
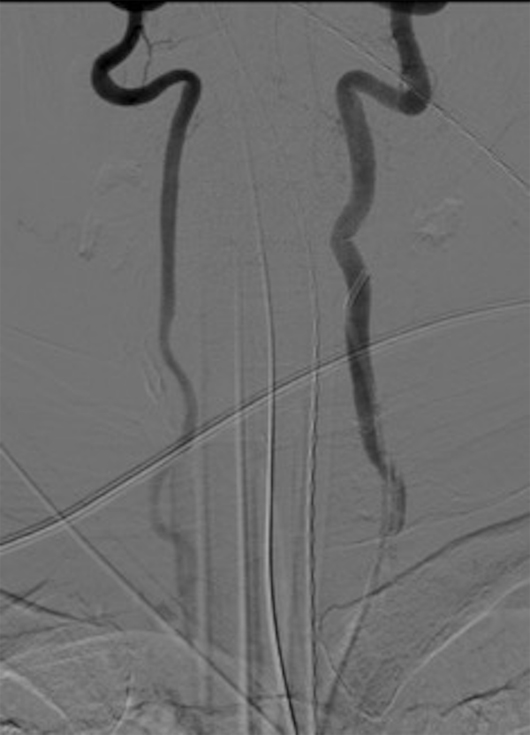
Figure 4

Figure 5
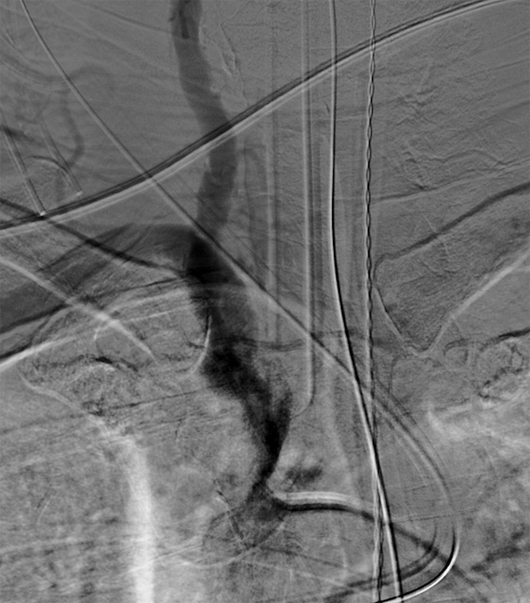
Figure 6

Figure 7
Diagnosis
Right subclavian steal syndrome (SSS).
Discussion
The innominate artery—or brachiocephalic artery—is the first branch of the aortic arch and supplies blood to the right arm and the head and neck. It divides into the right common carotid artery and the right subclavian artery.
SSS is characterized by hemodynamically significant stenosis or occlusion of the subclavian artery proximal to the origin of the vertebral artery or the innominate artery and is associated with retrograde flow through the ipsilateral vertebral artery.
While some patients remain asymptomatic, others, due to the steal phenomenon, may experience decreased blood flow to the posterior circulation resulting in vertebrobasilar insufficiency—ie, ataxia or vertigo—or arm pain during exercise. In such a scenario, SSS can be suspected with a difference in arm-to-arm blood pressure.
Symptoms in the setting of SSS indicate the compromise of distal perfusion to the vertebral artery or axillary artery. Hemodynamically, if the pressure distal to the subclavian artery stenosis/occlusion falls below a certain threshold, the pressure gradient will favor reversed blood flow through the ipsilateral vertebral artery.
Imaging modalities available to evaluate for SSS include Doppler ultrasound evaluation, which has no radiation, is usually readily available, and is fairly inexpensive. Available cross-sectional imaging such as CT and MRI can be considered when the etiology of the subclavian artery stenosis is unclear or for treatment planning.
In the absence of symptoms, no revascularization therapy is indicated. Symptomatic patients, however, can either be treated medically if symptoms are mild or, in the setting of severe symptoms, by vascular surgery or neurointerventional radiology. The procedural goal is to restore normal antegrade blood flow through the vertebral artery.
— Anna Luisa Kuhn, MD, PhD, is a radiologist in the department of radiology at UMass Memorial Medical Center.
— Ajit S. Puri, MD, is a radiologist in the department of radiology at UMass Memorial Medical Center.
Resources
1. Potter BJ, Pinto DS. Subclavian steal syndrome. Circulation. 2014;129(22):2320-2323.
2. Alcocer F, David M, Goodman R, Jain SK, David S. A forgotten vascular disease with important clinical implications. Subclavian steal syndrome. Am J Case Rep. 2013;14:58-62.
3. Sahsamanis G, Vourliotakis G, Pirgakis K, et al. Primary stenting of right-sided subclavian artery stenosis presenting as subclavian steal syndrome: report of 3 cases and literature review. Ann Vasc Surg. 2018;48:254.e1-254.e5.

