 On the Case
On the Case
By Pramod Gupta, MD
Radiology Today
Vol. 20 No. 12 P. 30
History
A 32-year-old woman presented to the emergency department with moderate-intensity, right-sided abdominal pain. She reported feeling mild pain occasionally for the past few weeks while running and lifting weights. The patient also reported that her pain had gradually worsened over the last two weeks. Her menstrual cycles were regular, and she had an uneventful past medical history. All routine laboratory tests were within normal limits, and a pregnancy test was negative. On physical examination, the patient had mild diffuse rebound tenderness. CT of the abdomen and pelvis was ordered. MRI of the pelvis was then obtained to further characterize the CT findings.
Findings
Axial and coronal CT images (Figures 1 and 2) demonstrate a cystic mass with an associated follicle consistent with significant enlargement of the right ovary (yellow arrow). T2-weighted axial (Figure 3) and postcontrast coronal and sagittal T1-weighted MR images (Figures 4 and 5) demonstrate several small nonenhancing follicles at the periphery of the significantly enlarged edematous T2 hyperintense right ovary (yellow arrow). There is associated mass effect on the uterus, which contains a very large degenerating subserosal fibroid, labeled “F” (Figure 5). Surgical detorsion of the ovary was successfully performed and confirmed the diagnosis.

Figure 1
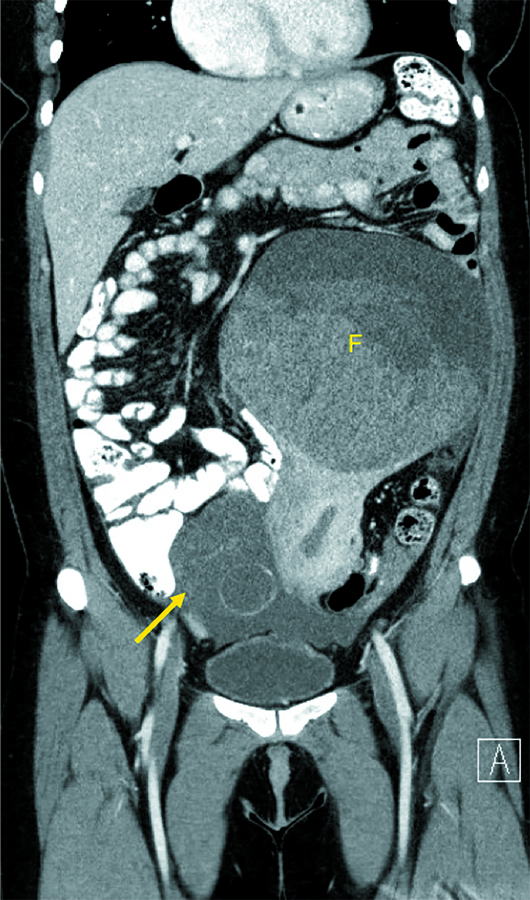
Figure 2
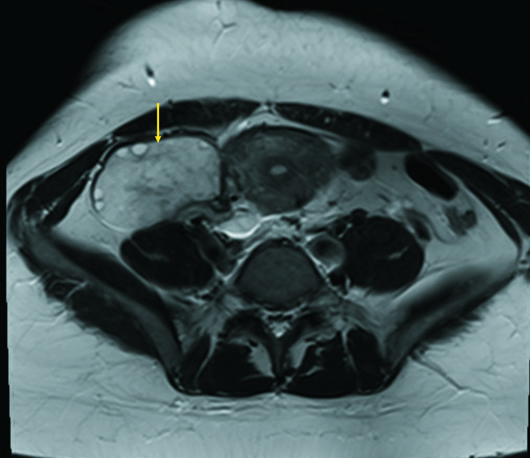
Figure 3
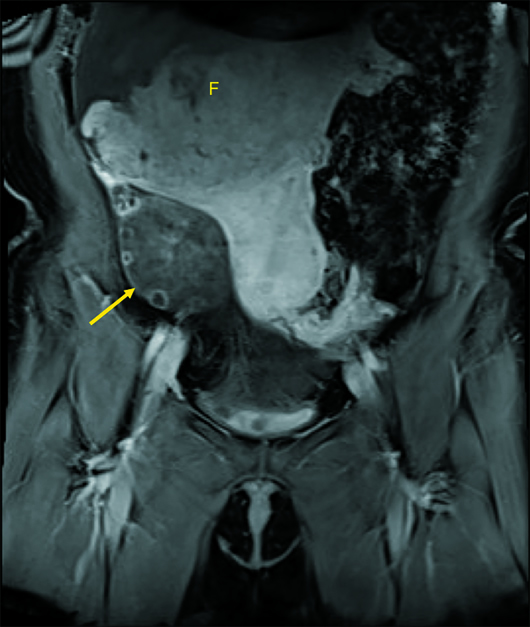
Figure 4
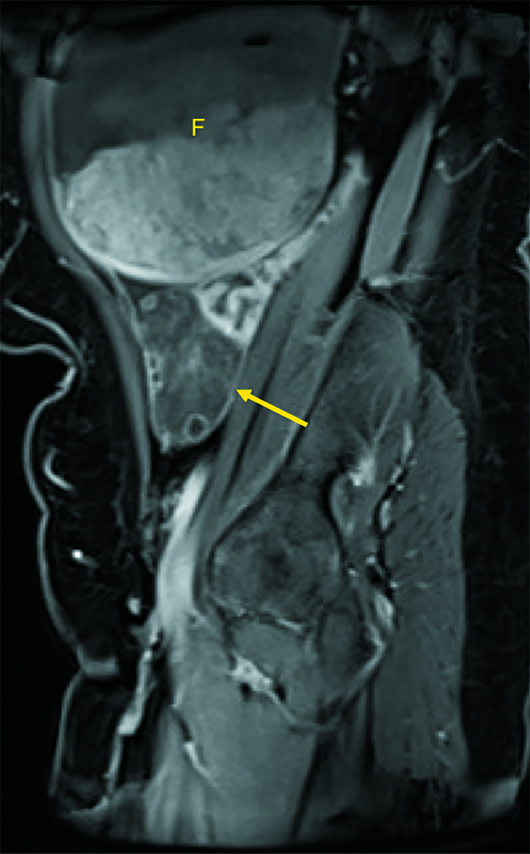
Figure 5
Diagnosis
Massive ovarian edema (MOE).
Discussion
MOE is a rare disease occurring in young women characterized by tumorlike enlargement of the ovary secondary to accumulation of interstitial fluid within the ovarian stroma. MOE can occur primarily in a normal ovary or secondarily in a previously diseased ovary usually containing a benign ovarian mass. Secondary massive ovarian edema is associated with many conditions including ovarian and intra-abdominal fibromatosis, Meig syndrome, ovarian mucinous or serous cystadenoma, mature cystic teratoma, polycystic ovaries, ovarian lymphatic dysfunction, and drugs used for ovarian induction. Some pathologists believe that MOE and fibromatosis may represent the same pathological process and exist along a continuum.
MOE most often affects women in their second and third decades, although it may occur at any age, including infancy. The majority of cases present with intermittent abdominal pain or a palpable mass. Menstrual irregularities and infertility are known associations. Occasionally, virilization and precocious puberty are the presenting symptoms, which may be the result of stimulatory changes that occur in stromal cells.
It has been suggested that MOE results from interference with the venous and lymphatic flow but not arterial blood flow, due to partial or complete torsion of the mesovarium. MOE is nearly always unilateral, and the right side is involved in two-thirds of the cases. The preponderance of right-sided involvement is attributed to higher pressure in the right ovarian vein compared with the left, since it drains directly into the inferior vena cava.
The pathognomonic findings of MOE are multiple follicles situated at the periphery of an enlarged ovary, associated with severe stromal edema on ultrasound or MRI. In some cases, large mature follicles may also be observed.
Findings on ultrasound include tumorlike enlargement of the ovary or hypoechoic ovarian enlargement with increased through transmission and peripherally displaced follicles. CT findings are typically nonspecific and include an enlarged edematous ovary with Hounsfield units <40, ipsilateral deviation of the uterus, and an edematous ipsilateral fallopian tube.
On MRI, solid tumorlike enlargement of the ovary is seen with hyperintensity on T2 with multiple peripheral follicles. Hemorrhage within the ovarian stroma may be seen as T1 hyperintensity and T2 hypointensity. Other findings include diffuse heterogeneous stromal enhancement, follicular wall enhancement, and a swollen, corkscrewlike fallopian tube.
Ovarian torsion can have a similar imaging appearance to MOE, but the presence of arterial waveforms on spectral Doppler and the presence of stromal and capsular enhancement on MRI favor a diagnosis of MOE. The pain of MOE is usually milder, chronic, and intermittent compared with the typical severe pain with acute/subacute ovarian torsion.
MOE can pose a significant clinical challenge, as it can be easily mistaken for a neoplasm, which can lead to overtreatment with resultant loss of hormonal function and fertility. If recognized, the patient can be treated with detorsion, wedge resection (removal of >30% of the ovarian volume), and plication of the ovary, resulting in preservation of ovarian function. When imaging is ambiguous, tumor markers such as beta-HCG, lactic dehydrogenase, CA-125, and alpha-fetoprotein can be used to narrow the differential. An intraoperative frozen section can also be used to assist in performing fertility-sparing surgery.
— Pramod Gupta, MD, is a staff radiologist at the Dallas VA Medical Center.
Resources
1. Hall BP, Printz DA, Roth J. Massive ovarian edema: ultrasound and MR characteristics. J Comput Assit Tomogr. 1993;17(3):477-479.
2. Lee AR, Kim KH, Lee BH, Chin SY. Massive edema of the ovary: imaging findings. AJR Am J Roentgenol. 1993;161(2):343-344.
3. Geist RR, Rabinowitz R, Zuckerman B, et al. Massive edema of the ovary: a case report and review of the pertinent literature. J Pediatr Adolesc Gynecol. 2005;18(4):281-284.
4. Yamashiro T, Inamine M, Kamiya H, Kinjo A, Murayama S, Aoki Y. Massive ovarian edema with torsion: unusual hemorrhage and the recovery of contrast enhancement. Emerg Radiol. 2008;15(2):115-118.
5. Umesaki N, Tanaka T, Miyama M, Kawamura N. Sonographic characteristics of massive ovarian edema. Ultrasound Obstet Gynecol. 2000;16(5):479-481.

