 Billing and Coding: The Talk of the Town
Billing and Coding: The Talk of the Town
By Melody W. Mulaik, MSHS, CRA, RCC, RCC-IR, CPC, COC, FAHRA
Radiology Today
Vol. 22 No. 1 P. 26
It’s time to brush up on E/M guidelines.
As we head into 2021, the biggest coding change being discussed in most radiology practices is the revision of the evaluation and management (E/M) guidelines. These revisions have changed how visit levels are assigned and also impact the reimbursement of other services to meet the budget neutrality requirement of their implementation. Radiologists will see an estimated 10% decrease in their overall Medicare reimbursement. These factors are driving practices to review new opportunities to bill for E/M services. While the guidelines have not changed for inpatient E/M codes, now is a good time to look for opportunities in all places of service.
In short, the changes for 2021 include the deletion of 99201 (new patient visit level 1), creation of two new add-on codes for extended visits (99417 and G2212), elimination of history and/or physician exam in determining the billable code level, and code assignment for new (99202–99205) and established (99211–99215) patient visits based on time or medical decision making (MDM).
The American Medical Association (AMA) indicates that the definition of time is the minimum time—not the typical time—and represents total physician/qualified health care professional (QHP) time on the date of service. The use of these codes requires a face-to-face encounter by the physician or other QHP and includes the total of face-to-face and non–face-to-face time. The total time does not include time for activities normally performed by clinical staff. A QHP is defined as an individual who, by education, training, licensure/regulation, and facility privileging, can perform a professional service within his/her scope of practice and independently report a professional service for reimbursement. If the visit is a split/shared visit, only distinct time should be summed when two or more individuals meet with or discuss the patient so that only the time of one individual is counted.
If more than one billing practitioner sees the patient as part of the encounter on the date of service, only one person is counted per minute of time applied to the billable level. To count the time of multiple practitioners would be “double dipping” related to time. Each level of visit will now have an assigned range of time to better identify the appropriate level of service per the documented work of the encounter.
If time is selected, there is no minimum amount of MDM that must also be documented in the note. However, there is basic documentation needed to be considered a credible visit for billing purposes. Typical activities that can be used toward total time include: preparing to see the patient, eg, review of tests; counseling and education for the patient/family/caregiver; documenting clinical information in the EHR; obtaining and/or reviewing separately obtained history; ordering medications, tests, or procedures; independently interpreting results—not separately reported—and communicating results to patients/families/caregivers; performing a medically appropriate examination and/or evaluation; referring and communicating with other health care professionals, when not separately reported; and care coordination, not separately reported.
The following tables identify the time ranges assigned to each level of new and established patient visits beginning in 2021.
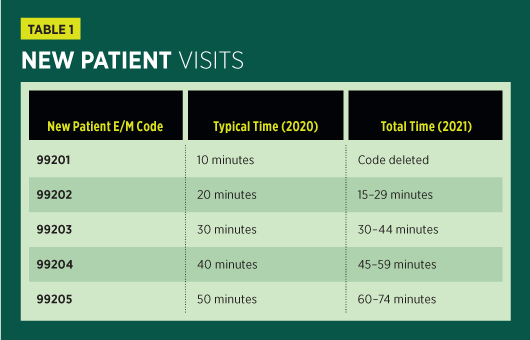
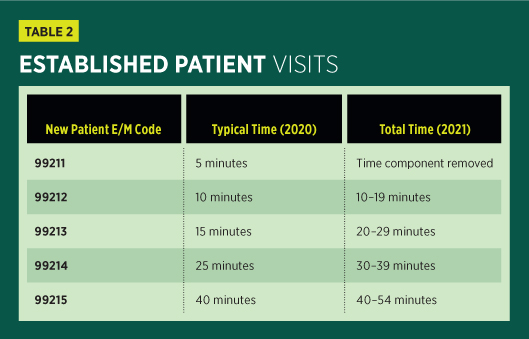
There may be instances in which the time spent with the patient during outpatient E/M encounter will run longer than the allotted time of 74 minutes for a new patient (99205) or 54 minutes for an established patient (99215). Beginning January 1, 2021, new prolonged services codes are available for use with the revised outpatient and office visit codes.
The new code by the AMA and for use with payers, except Medicare, is CPT 99417, and it replaces the previously used codes 99358 and 99359. Codes 99358 and 99359 are still valid in 2021, but they are no longer billable with the revised outpatient E/M service codes. The newly created code is billable with time-based reporting for office/outpatient visit codes that have reached the threshold for a level 5 visit (99205 and 99215). The Centers for Medicare & Medicaid Services opted to not utilize 99417 and instead created the HCPCS add-on code G2212.
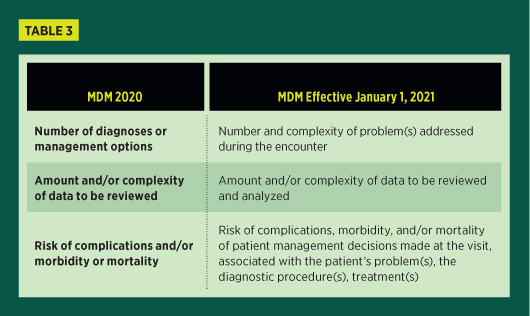
If medical decision making is the selected method for documentation, there are changes to the criterion to support the levels of outpatient and office E/M services. There will continue to be four levels of MDM; this is unchanged from the levels used in 2020: straightforward, low, moderate, and high.
The corresponding billable level of MDM will continue to be based on two of the following three elements, as defined by the AMA:
• number and complexity of problems addressed at the encounter;
• amount and/or complexity of data to be reviewed and analyzed; and
• risk of complications and/or morbidity or mortality of patient management.
Even though the documentation of the patient history and examination will no longer be applied when determining the level of the outpatient visit, it is still expected that the documentation will include these components as medically appropriate to the visit. For outpatient visits, the history tells an important story about the patient, and the examination may provide additional details necessary to the course of care.
To understand the changes to MDM for outpatient E/M visits, the following table compares the criteria as they were in 2020 to the new criteria in 2021.
If the problem is scheduled for further testing; cannot be treated due to risk to the patient; or the patient, parent, or guardian elects not to be treated, this is considered addressing the problem. If the document supports that another physician is managing the patient for the problem and there is no evaluation of that problem, this will not count. The same would be true if the patient was referred for evaluation of a problem but was not evaluated or the problem was not considered for treatment.
According to CPT Assistant, when selecting the level of outpatient E/M visit, comorbidities/underlying diseases are not part of the consideration in the billable level, unless they are addressed as part of the encounter and they increase the amount/complexity of data reviewed and analyzed or they increase the risk of complications and/or morbidity or mortality related to the management of the patient.
In addition, utilization of the MDM method to document and bill an appropriate E/M visit requires the billing physician to understand key terminology specific to the MDM criterion. The AMA has provided descriptions to align the level of MDM with examples of each.
Now is a good time to review the current opportunities to bill for E/M services and implement appropriate processes to ensure adequate documentation and accurate billing.
— Melody W. Mulaik, MSHS, CRA, RCC, RCC-IR, CPC, COC, FAHRA, is the president of Coding Strategies, Inc, and Revenue Cycle, Inc.

