 On the Case
On the Case
By Ryan Johnson, DO; Daniel Maloney, DO; Min-Chul Shin, MD; and Ryan Chapman
Radiology Today
Vol. 24 No. 1 P. 32
History
A 73-year-old man with a past medical history of atrial fibrillation presented to the hospital with heartburn, shortness of breath, and chills. His clinical symptoms started after he underwent a pulmonary vein ablation procedure one month earlier for uncontrolled atrial fibrillation. CT imaging of the chest was performed to further evaluate for ablation-related complications, given the patient’s symptoms and recent history of pulmonary vein ablation. His hospital course was subsequently complicated by septic shock, endocarditis, and stroke.
Findings
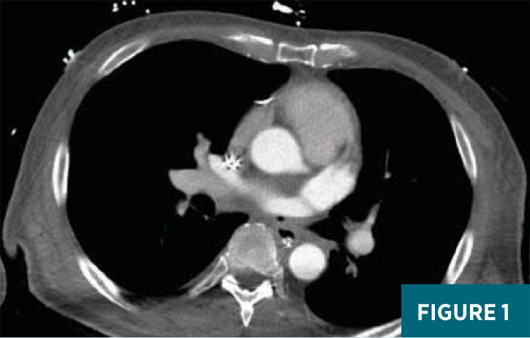
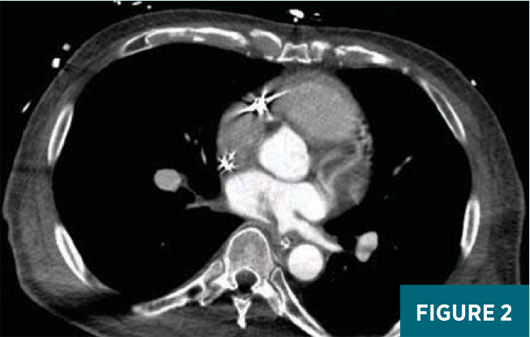
A contrast-enhanced axial CT image at the level of the superior aspect of the left atrium (Figure 1) demonstrated a small focus of air density abutting the posterior wall of the left atrium. This was extraluminal to the esophagus. A contrast-enhanced axial CT image slightly inferior to Figure 1, at the level of the mid-left atrium (Figure 2), demonstrated a soft tissue density with a feathered edge arising from the posterior wall of the left atrium extending into the left atrial cavity. A contrast-enhanced oblique reformatted CT image (Figure 3) demonstrated a small focus of extraluminal air adjacent to the esophagus and abutting the posterior wall of the left atrium with a “wispy” soft tissue density extending into the left atrium.
Given the patient’s recent history of pulmonary vein ablation along with the CT imaging findings, he was diagnosed with an atrioesophageal fistula with a left atrial thrombus.

Diagnosis
Ablation-related atrioesophageal fistula (AEF)
Discussion
Atrial fibrillation is the most common sustained cardiac arrhythmia, a major cause of stroke, and the most common cardiac arrhythmia requiring hospitalization. Atrial fibrillation originates from the atria and usually begins as paroxysmal atrial fibrillation, with approximately 60% of patients converting spontaneously to a normal sinus rhythm. Approximately 40% of patients develop persistent atrial fibrillation requiring medical or procedural intervention to restore normal sinus rhythm. Up to 50% of patients develop recurrent atrial fibrillation.
Arrhythmogenic foci originating within the pulmonary veins are an important cause of both paroxysmal and persistent atrial fibrillation. A variety of surgical and endovascular techniques have been used to electrically disconnect the pulmonary veins from the left atrium.
AEF has become a recognized severe complication of ablative therapies for atrial fibrillation due to the close proximity of the anterior esophageal wall to the posterior aspect of the left atrium.1 The exact mechanism involved in AEF formation is unknown; however, there have been multiple proposed theories and, perhaps, the mechanism is not a single factor but a combination of factors. Mucosal damage is thought to occur secondary to thermal injury from radioablation. It has been shown that higher ablation temperatures, power, and larger nonirrigated catheters have been associated with the development of AEFs.2 Thermal damage may also affect the anterior esophageal arteries leading to ulcerations. Damage to vagal fibers may impair the lower esophageal sphincter tone, which in turn increases gastroesophageal reflux, further worsening mucosal damage at the site of ablation. Lastly, esophageal dysmotility is thought to occur from general anesthesia leading to impaired swallowing and altered peristalsis, which worsens the mucosal insult.3
Additional catheter ablation-associated complications include cardiac tamponade, stroke, venous thromboembolism, myocardial infarction, pneumonia, and sepsis.3 AEF is the rarest complication of pulmonary vein ablation, occurring in approximately 0.1% to 0.25% of patients, and is associated with the highest mortality rate.3-5
Esophageal perforation is usually detected within one to five weeks after ablation, and patients tend to present with chest pain, dysphagia, heartburn, fever, malaise, neurological symptoms, and hematemesis.1 The fistula between the esophagus and the left atrium can lead to sepsis from upper gastrointestinal tract bacteria, ischemic neurological deficits from air emboli, and melena from massive upper gastrointestinal bleeding.6
This case of AEF associated with pulmonary vein ablation demonstrates the importance of thoroughly assessing the mediastinum, including the left atrium and esophagus, for subtle findings in patients who have recently undergone catheter ablation for atrial fibrillation. Due to the wide range of presenting symptoms, which may be vague, a high degree of clinical concern and communication with the radiologist is prudent in making the diagnosis.
Ryan Johnson, DO, is a diagnostic radiology resident at ChristianaCare in Newark, Delaware.
Daniel Maloney, DO, is a staff radiologist at ChristianaCare.
Min-Chul Shin, MD, is a staff radiologist at ChristianaCare.
Ryan Chapman is a medical student at Touro College of Osteopathic Medicine in Middletown, New York.

