 On the Case
On the Case
By Alexis Cammarata, DO; Alejandro Garces, MD; Min-Chul Shin, MD; and Daniel Maloney, DO
Radiology Today
Vol. 24 No. 2 P. 30
History
A 57-year-old man initially presented to an urgent care center with a history of acute on chronic intermittent abdominal pain. The patient was referred for CT imaging, which revealed cholelithiasis without secondary signs of acute cholecystitis. The patient was referred to general surgery but declined to follow up due to the COVID-19 pandemic. Approximately one year later, the patient had an acute recurrent bout of severe abdominal pain, presented to the emergency department (ED), and had CT imaging of the abdomen and pelvis and, subsequently, an MRI of the abdomen.
Findings
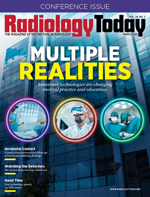
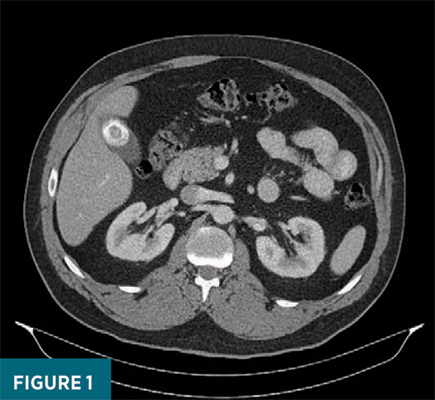
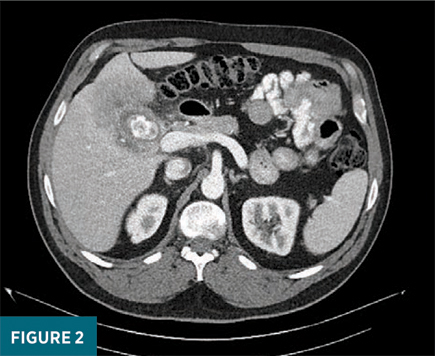
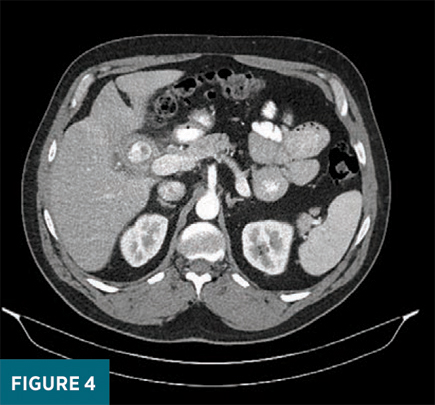
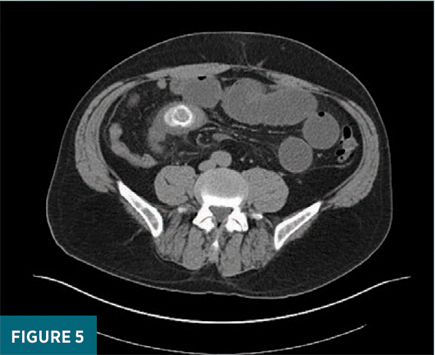
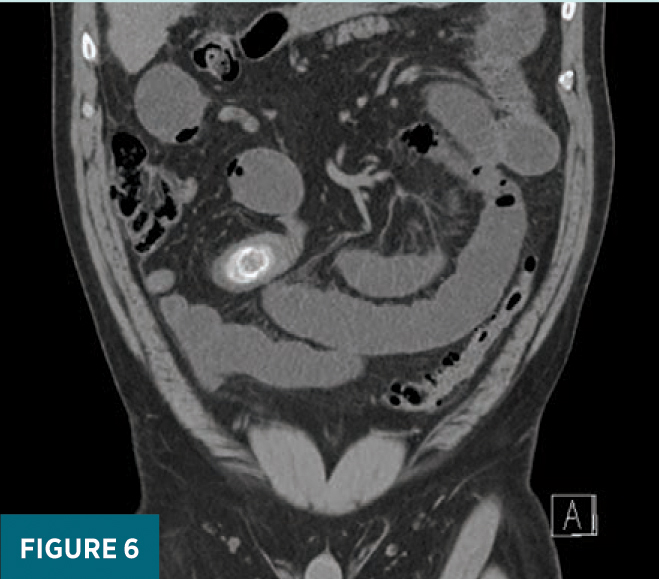
Contrast-enhanced axial CT images of the abdomen demonstrated a 2.9 cm gallstone within the gallbladder (Figure 1). A second, slightly larger, intraluminal gallstone was noted near the gallbladder neck with associated irregular gallbladder wall thickening, adjacent fat stranding, and heterogeneous low-attenuation of the hepatic parenchyma bordering the gallbladder fossa (Figure 2). There was also an enlarged, morphologically abnormal, lymph node in the vicinity of the gallbladder. CT findings were most consistent with acute on chronic cholecystitis, but the possibility of gallbladder carcinoma (GBC) was also raised. Contrast- enhanced MRI of the abdomen was subsequently performed and redemonstrated a large gallstone within the contracted gallbladder with extensive gallbladder wall thickening and substantial heterogeneous hyperenhancement of the adjacent hepatic parenchyma (Figure 3). The patient then underwent an endoscopic biopsy of the morphologically abnormal lymph node to rule out GBC, but the pathology result was inconclusive. The decision was made for short term imaging follow up. On follow up contrast-enhanced CT, persistent wall thickening of the contracted gallbladder with a dominant gallstone near the neck was again noted; however, the previously noted heterogeneous enhancement of the adjacent liver parenchyma had improved (Figure 4). Clinically, the patient was also showing signs of improvement while awaiting definitive outpatient cholecystectomy. Before his surgery, the patient again developed acute severe abdominal pain and bloating, which led him to the ED with noncontrast CT imaging demonstrating an interval passage of the previously noted gallstone into the lumen of the ileum, resulting in a small bowel obstruction (Figures 5 and 6). These findings were consistent with the diagnosis of gallstone ileus with associated pneumobilia. The patient was subsequently taken to the operating room and had a partial small bowel resection of the ileum. Pathology showed the small intestine with acute ischemic changes and an impacted gallstone.
Diagnosis
Gallstone ileus in the setting of chronic cholecystitis
Discussion
Chronic cholecystitis is an inflammatory condition of the gallbladder secondary to functional or mechanical dysfunction of bile emptying. Radiological findings associated with chronic cholecystitis include the presence of a gallstone, increased attenuation of bile, and significant wall thickening secondary to prolonged inflammation.1 Untreated chronic cholecystitis may result in the formation of a cholecystoenteric fistula, with subsequent passage of the gallstone through the fistula into the bowel, leading to a mechanical bowel obstruction. Gallstone ileus is a rare complication of cholelithiasis and is one of the rarest forms of mechanical bowel obstruction. Patients typically present four to eight days after symptoms start. The diagnosis is often delayed since symptoms may be intermittent. As a result, gallstone ileus continues to be associated with relatively high rates of morbidity and mortality.
The etiology of gallstone ileus results from adhesions forming between an inflamed gallbladder and an adjacent gastrointestinal tract, followed by gallstones causing pressure necrosis or inflammation, which results in erosion and formation of a cholecystoenteric fistula. Fistulas can form within any part of the gastrointestinal tract, with approximately 60% occurring in the duodenum due to its proximity. The site of fistula formation, size of the gallstone, and size of the bowel lumen will determine the location of impaction. Gallstones most commonly impact the terminal ileum and ileocecal valve due to their narrow lumen and less active peristalsis. The majority of gallstones smaller than 2 cm may pass spontaneously, while those larger are more likely to become impacted.
GBC is the fifth most common gastrointestinal neoplasm, with a dismal five-year survival rate of 5% to 12% with local spread to multiple hepatic segments.2-4 Early detection and prompt surgical treatment can increase the five-year survival rate to up to 75%.3 GBC imaging characteristics on CT and MRI may demonstrate an intraluminal mass lesion, focal or diffuse asymmetrical wall thickening, or an intraluminal polyp.5 However, these findings may be subtle.
GBC and chronic cholecystitis carry many similarities on imaging, which include gallbladder wall thickening and, in this case, hyperenhancement of the adjacent liver. It was not until the patient had a biopsy of the morphologically abnormal lymph node and subsequent improvement on imaging that GBC was adequately ruled out.
On CT, findings consistent with gallstone ileus include gallbladder wall thickening, pneumobilia, intestinal obstruction, and obstructing gallstones. Pneumobilia, a nonspecific finding, is found in approximately 30% to 60% of patients. A hepatobiliary iminodiacetic acid scan, MR cholangiopancreatography, and esophagogastroduodenoscopy may be performed if there is still a question after CT imaging. However, gallstone ileus is more typically diagnosed intraoperatively when a patient is undergoing laparotomy for small bowel obstruction of unknown origin.
Alexis Cammarata, DO, is a diagnostic radiology resident at ChristianaCare in Newark, Delaware.
Alejandro Garces, MD, is a diagnostic radiology resident at ChristianaCare.
Min-Chul Shin, MD, is a staff radiologist at ChristianaCare.
Daniel Maloney, DO, is a staff radiologist at ChristianaCare.

