 On the Case
On the Case
By Brad Kincaid, MD; Fatima Khan, BS; and Alex Merkulov, MD
Radiology Today
Vol. 21 No. 9 P. 28
History
A 56-year-old woman with a history of phyllodes tumor (PT) in the left breast presented with a new palpable left breast mass. Her breast-related history is extensive. Bilateral breast implants were placed in 2009. In 2013, the patient had a left breast excisional biopsy for a concerning mass, and pathology identified a cellular fibroadenoma with epithelial ductal hyperplasia. In 2015, an additional palpable left breast mass was evaluated and consistent with high-grade PT. She underwent a skin-sparing left mastectomy. Postsurgical pathology revealed two separate high-grade PTs measuring 6 cm and 3 cm with negative margins. Radiation therapy was not performed.
In 2020, five years after initial resection, the patient again appreciated a left breast mass on self-examination and appropriate work-up was initiated.
Findings
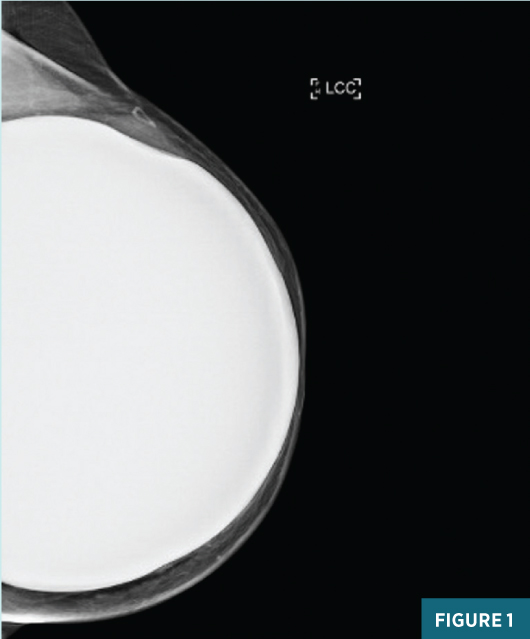
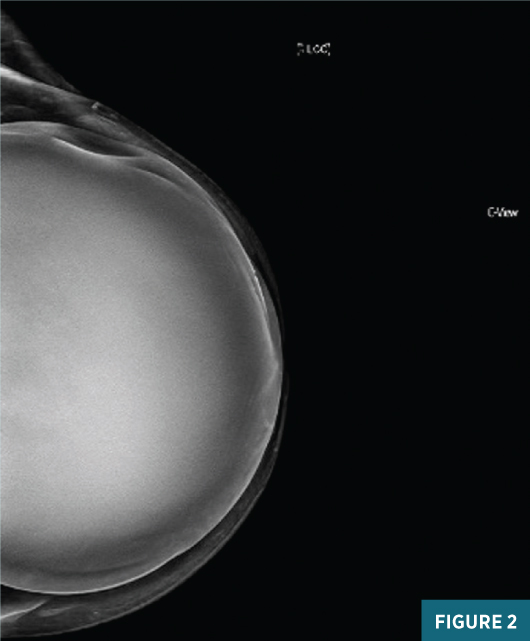
A diagnostic left breast mammogram with full-field 2D and C-View 2D digital images (Figures 1 and 2) reveals an equal-density 2.1 cm lateral mass with associated indentation of the left breast implant. A skin marker denotes the palpable abnormality. There are no suspicious associated calcifications. Concurrent targeted breast ultrasound (Figures 3 and 4) demonstrates a 2.4 cm, 2:00, 9 cm from nipple parallel solid hypoechoic circumscribed mass centered between the dermis and the breast implant, with faintly detectable internal vascularity.
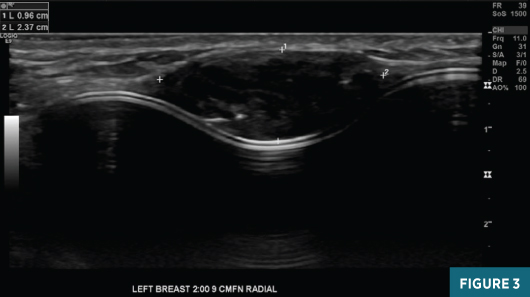
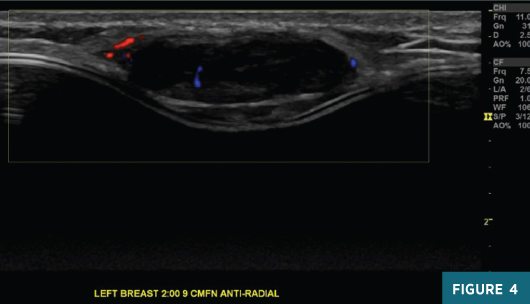
Sonographic features were suspicious for malignancy and an ultrasound-guided needle biopsy was performed; pathology results were most consistent with malignant PT. The patient underwent left breast partial mastectomy with removal of the left breast implant. Postoperative pathology results confirmed a recurrent malignant PT. After consultation with the radiation oncologist and given the recurrent disease, the patient opted to pursue postsurgical radiation therapy.
Diagnosis
Recurrent malignant PT.
Discussion
PT is a rare fibroepithelial neoplasm of the breast with the ability to grow and metastasize.1 These neoplasms are slow growing, painless, and classically detected in the upper outer quadrant of the breast.2 PT accounts for <1% of all breast tumors and 2% to 3% of all fibroepithelial breast lesions.3 It typically occurs in women aged 30 to 70 years, with average presentation at 52 years.4 On histology, PT has a characteristic leaflike architecture with epithelial papillary projections into cystic spaces and a hypercellular stroma.5 In fact, the name phyllodes is derived from the Greek word phullon, meaning “leaf,” which reflects its histologic characteristics.
Imaging findings of PT often resemble that of a fibroadenoma.4 On mammography, PT appears as a large, circumscribed, lobulated mass without calcifications.6 Sonographic evaluation demonstrates a well-defined lobulated mass, often with a pseudocapsule and fluid-filled clefts with internal echogenic elements. In general, a solid mass with multiple cleftlike cystic spaces with increased through transmission is the typical appearance and should raise the question of PT. Doppler evaluation may demonstrate vascularization within the solid components of the mass, though Doppler has variable sensitivity.1 MRI may also be used to evaluate PT and usually reveals a T2 hyperintense oval-shaped, lobulated, circumscribed mass with rapid enhancement after contrast administration.7 Overall, imaging characteristics are quite nonspecific, and the differential diagnosis usually includes fibroadenoma or primary sarcoma of the breast.8
The treatment of PT is surgical excision with wide margins to avoid recurrence of both benign and malignant tumors. Despite this, local recurrence is observed in up to 25% of cases. Malignant tumors are detected in 5% to 25% of PT cases, with up to 25% being metastatic. Metastatic PT can spread hematogenously to the lungs, pleura, or bones.7 Mastectomy may be performed for very large or recurring malignant PT.9
— Brad Kincaid, MD, is a radiology resident at UConn Health at the University of Connecticut.
— Fatima Khan, BS, is a fourth-year medical student at Frank H. Netter School of Medicine at Quinnipiac University in North Haven, Connecticut.
— Alex Merkulov, MD, is an associate professor of radiology at UConn Health.
References
1. McCarthy E, Kavanagh J, O'Donoghue Y, McCormack E, D'Arcy C, O'Keeffe SA. Phyllodes tumours of the breast: radiological presentation, management and follow-up. Br J Radiol. 2014;87(1044):20140239.
2. Reinfuss M, Mituś J, Duda K, Stelmach A, Ryś J, Smolak K. The treatment and prognosis of patients with phyllodes tumor of the breast: an analysis of 170 cases. Cancer. 1996;77(5):910-916.
3. Rowell MD, Perry RR, Hsiu JG, Barranco SC. Phyllodes tumors. Am J Surg. 1993;165(3):376-379.
4. Farria DM, Gorczyca DP, Barsky SH, Sinha S, Bassett LW. Benign phyllodes tumor of the breast: MR imaging features. AJR Am J Roentgenol. 1996;167(1):187-189.
5. Sewell CW. Pathology of benign and malignant breast disorders. Radiol Clin North Am. 1995;33(6):1067-1080.
6. Liberman L, Bonaccio E, Hamele-Bena D, Abramson AF, Cohen MA, Dershaw DD. Benign and malignant phyllodes tumors: mammographic and sonographic findings. Radiology. 1996;198(1):121-124.
7. Lifshitz OH, Whitman GJ, Sahin AA, Yang WT. Radiologic-pathologic conferences of the University of Texas M.D. Anderson Cancer Center. Phyllodes tumor of the breast. AJR Am J Roentgenol. 2003;180(2):332.
8. Wurdinger S, Herzog AB, Fischer DR, Marx C, Raabe G, Schneider A, Kaiser WA. Differentiation of phyllodes breast tumors from fibroadenomas on MRI. AJR Am J Roentgenol. 2005;185(5):1317-1321.
9. Salvadori B, Cusumano F, Del Bo R, Delledonne V, Grassi M, Rovini D, Saccozzi R, Andreola S, Clemente C. Surgical treatment of phyllodes tumors of the breast. Cancer. 1989;63(12):2532-2536.

