 On the Case
On the Case
By David Baltrusaitis, MD, and Alex Merkulov, MD
Radiology Today
Vol. 24 No. 6 P. 30
History
A 36-year-old pregnant woman, with a gestational age of 24 weeks and one day, was evaluated for interval fetal growth by maternal- fetal medicine and referred for MRI imaging. Her pregnancy was complicated by placenta previa based on ultrasound imaging performed at 19 weeks gestation.
Findings
MRI of the abdomen and pelvis without IV contrast revealed the following:
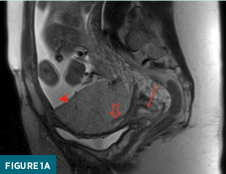
A T2 weighted sagittal image of a gravid uterus demonstrates placenta previa and accreta. A homogenous placenta overlies the cervix. A thick T2 hypointense band is noted. The fetus is in breach position (Figure 1a).
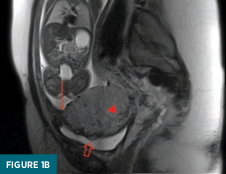
An abnormal placental-myometrial interface with an obscured inner uterine layer and thinning of the myometrium is noted. The placenta extends to the urinary bladder interface, which demonstrates nodular contour and flow voids. The posterior aspect of the aforementioned hypointense band is noted dorsally (Figure 1b).
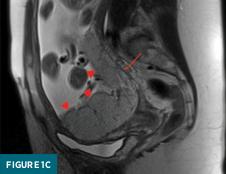
Extension of the placenta along the posterior surface of the uterus exhibits a smooth, contiguous placental-myometrial interface (Figure 1c).
Ultrasound correlation demonstrated the following:
Greyscale transabdominal sonographic examination of the uterus shows a placenta with lacunae. There is loss of the normal retroplacental clear space. The hyperechoic placenta extends to the interface with the urinary bladder with obscuration of the normal hyperechoic line separating the uterus from the urinary bladder. Note the posterior placenta is obscured on this exam (Figure 2a).

Transabdominal power doppler of the uterus demonstrates a hyperechoic placenta extending to and creating a nodular interface with the urinary bladder, obscuring the normal hyperechoic line separating the uterus from the urinary bladder (Figure 2b).

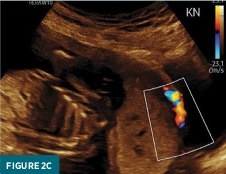
Power Doppler exam demonstrates hypervascularity at the placental-vesicular interface (Figure 2c).
Diagnosis
Placenta previa and accreta.
Discussion
Recognizing abnormal placental positioning and attachment to the uterus during pregnancy is a crucial skill for general radiologists. A firm understanding of the normal uterus and placenta is needed to identify the abnormal.
The general shape of the gravid uterus typically demonstrates morphology akin to an inverted pear with smooth surface contours. During sonographic evaluation, the placenta should show homogenously intermediate echotexture. The bladder, in comparison, should have a relatively hyperechoic mucosa. Placental position is considered normal when located anteriorly, posteriorly, left, right, or at the fundus of the uterine body.1 The edge of the placenta should be located at greater than 2 cm away from the internal cervical os, and the umbilical cord should insert into the center of the placenta.2
If the placental margin is less than 2 cm from the internal cervical os, the term low-lying placenta may be invoked. The diagnosis of placenta previa is met when the placental edge covers the internal os. Recently, usage of the terms “partial” and “marginal” previa have been discouraged in favor of measuring the distance of the placental margin to the internal os, allowing for a more quantitative risk stratification of hemorrhage during delivery.3 As the placenta migrates approximately 1 mm per week, previa may resolve over the course of the pregnancy. This fact necessitates repeat imaging evaluations in the third trimester.
Retrospective studies have shown that the greatest risk for persistence of placenta previa is cases of complete coverage of the internal os and persistence of previa beyond the midpoint of pregnancy.4 Additionally, women with history of prior cesarian delivery were more likely to have persistent placenta previa compared with those who underwent vaginal delivery.
After fertilization, the blastocyte attaches to the endometrium, with differentiation of the outermost layer into syncytiotrophoblasts and cytotrophoblasts. 5 The placenta accreta spectrum describes the abnormal attachment of the placenta to the uterus, thought to be secondary to absent decidua at the site of implantation and abnormally excessive trophoblastic invasion.5 Variants of this disease process, ie, accreta, increta, and percreta, are differentiated by the depth of invasion. Accreta is defined by abnormal attachment to the myometrium. Increta is abnormal invasion into the myometrium. Percreta exhibits invasion up to or through the uterine serosa.2 Risk factors for the accreta spectrum include placenta previa, advanced maternal age, grandmultiparity, previous curettage, previous myomectomy, previous uterine surgery, submucosal myoma, Asherman’s syndrome, short C-section to conception interval, and female fetus.6
Ultrasound is most often the first, and often the primary, source of imaging in the setting of the placenta accreta spectrum, as most pregnancies undergo sonographic evaluation between gestational ages of 18 to 20 weeks. Pertinent findings frequently include loss of retroplacental clear space, reduced myometrial thickness, placental lacunae with turbulent Doppler flow, and irregular bladder wall surface contour.7 Visualization of lacunae has been cited as the highest sensitivity for diagnosis of placenta accreta.8
Utilization of MRI for this pathology has increased, most frequently in the setting of posteriorly implanted placenta or after encountering uncertain sonographic findings. MRI allows for the potential of increased accuracy in evaluating the depth of invasion, sensitivity in detecting extent of disease, and obtaining consistent uterine topography for comparisons between repeat evaluations.9 Furthermore, MRI allows for the division of the uterus into sectors distinguishing areas where the blood supply is accessible for emergent intervention in the case of hemorrhage vs regions less accessible secondary to anatomic depth or multisource blood supply.9 At minimum, the axial, sagittal, and coronal planes should be obtained with T2-weighted nonfat-suppressed sequences. To aid evaluation of abnormal attachment to the uterus, axial oblique T2 images should be obtained perpendicular to the placental-myometrial interface. 10 T1 fat-suppressed sequences may be used to identify placental hemorrhage or abruption. When able, breath-holding techniques and fast imaging technology should be employed to avoid motion artifacts from both the mother and fetus.3 Optional sequences include a steady-state free procession to evaluate anatomy and vasculature and diffusion-weighted imaging to aid in the topographic delineation of the placental margins.10
The normal placenta should have homogenously intermediate T2 signal with thin, regularly interspaced low-signal intraparenchymal septal bands. The uterine myometrium should have three layers: a thin outer hypointense layer, a middle thick layer of intermediate signal often containing flow voids, and a thin inner hypointense layer. Findings that raise the most suspicion for placenta accreta include heterogeneous signal within the placenta; uterine bulging, which disrupts the normal uterine contour; and thick T2 hypointense intraplacental bands.11 Assessing the myometrial-placental interface is of lesser importance with MRI as the border between these structures is often blurred.
The accurate and timely diagnosis of placenta previa and the accreta spectrum is imperative for guiding clinicians throughout a patient’s pregnancy. Specifically, in the case of placenta accreta, radiologists may help plan the site of delivery, blood products can be prepared prior to surgery in the anticipation of hemorrhage, and the appropriate subspecialists will be involved early in the diagnosis. C-section is typically planned at 36 weeks to avoid spontaneous delivery. A hysterectomy is indicated when there is excessive blood loss or if preservation of fertility is not desired. When a hysterectomy is not performed, less invasive management varies between institutions and includes leaving the placenta to eventually involute, localized resection and repair, oversewing a surgical defect, and blunt dissection/curettage.12
— David Baltrusaitis, MD, is a diagnostic radiology resident at UConn Health at the University of Connecticut.
— Alex Merkulov, MD, is an associate professor of radiology at UConn Health at the University of Connecticut.
References
1. Fadl S, Moshiri M, Fligner CL, Katz DS, Dighe M. Placental imaging: normal appearance with review of pathologic findings. Radiographics. 2017;37(3):979-998.
2. Elsayes KM, Trout AT, Friedkin AM, et al. Imaging of the placenta: a multimodality pictorial review. Radiographics. 2009;29(5):1371-1391.
3. Baughman WC, Corteville JE, Shah RR. Placenta accreta: spectrum of US and MR imaging findings. Radiographics. 2008;28(7):1905-1916.
4. Dashe JS, McIntire DD, Ramus RM, Santos-Ramos R, Twickler DM. Persistence of placenta previa according to gestational age at ultrasound detection. Obstet Gynecol. 2002;99(5, Pt 1):692-697.
5. Tantbirojn P, Crum CP, Parast MM. Pathophysiology of placenta creta: the role of decidua and extravillous trophoblast. Placenta. 2008;29(7):639-645.
6. Usta IM, Hobeika EM, Abu Musa AA, Gabriel GE, Nassar AH. Placenta previa-accreta: risk factors and complications. Am J Obstet Gynecol. 2005;193(3 Pt 2):1045-1049.
7. Comstock CH. Antenatal diagnosis of placenta accreta: a review. Ultrasound Obstet Gynecol. 2005;26(1):89-96.
8. Yang JI, Lim YK, Kim HS, Chang KH, Lee JP, Ryu HS. Sonographic findings of placental lacunae and the prediction of adherent placenta in women with placenta previa totalis and prior Cesarean section. Ultrasound Obstet Gynecol. 2006;28(2):178-182.
9. Palacios Jaraquemada JM, Bruno CH. Magnetic resonance imaging in 300 cases of placenta accreta: surgical correlation of new findings. Acta Obstet Gynecol Scand. 2005;84(8):716-724.
10. Jha P, Pōder L, Bourgioti C, et al. Society of Abdominal Radiology (SAR) and European Society of Urogenital Radiology (ESUR) joint consensus statement for MR imaging of placenta accreta spectrum disorders. Eur Radiol. 2020;30(5):2604-2615.
11. Lax A, Prince MR, Mennitt KW, Schwebach JR, Budorick NE. The value of specific MRI features in the evaluation of suspected placental invasion. Magn Reson Imaging. 2007;25(1):87-93.
12. You WB, Zahn CM. Postpartum hemorrhage: abnormally adherent placenta, uterine inversion, and puerperal hematomas. Clin Obstet Gynecol. 2006;49(1):184.
