 On the Case
On the Case
By Mina Botros, BS; Jasmeet Singh, MD; and Anna Luisa Kuhn, MD, PhD
Radiology Today
Vol. 25 No. 3 P. 24
History
A 38-year-old woman with a remote history of cocaine use and migraines presented unresponsive to the emergency department and then suffered a witnessed generalized tonic-clonic seizure. Leading up to the loss-of-consciousness event, she had been experiencing worsening headaches and left-sided weakness. Cross-sectional imaging was obtained on the patient with MRI and CT angiogram.
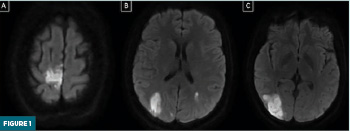
Findings
On axial diffusion-weighted MRI images demonstrate infarcts in the paramedian right posterior frontal lobe, bilateral parietal lobes, and parieto- occipital region (Figure 1A-C).
Axial maximum intensity projection CT angiogram image of the head at the level of the midbrain shows diffuse irregularities along the bilateral anterior and posterior circulation vessels, resulting in stenoses of varying degrees (Figure 2).

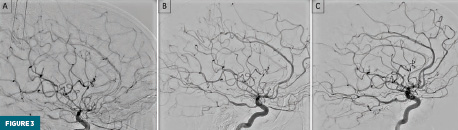
Lateral view digital subtraction angiography (DSA) of the right internal carotid artery (ICA) shows small caliber bilateral anterior cerebral artery (ACA) territories with diminished contrast opacification and some irregularities in the right middle cerebral artery territory (Figure 3A).
Lateral view DSA of the right ICA after slow intra-arterial infusion of a calcium channel blocker (verapamil) showed improvement in vessel caliber throughout the right anterior circulation with clear improvement of vessel caliber and contrast opacification of the bilateral ACAs. Some residual vessel irregularities remain in the proximal ACAs (Figure 3B).
Lateral view DSA of the right ICA three months after initial admission, at the time of an elective endovascular aneurysm repair, showed normal caliber of the intracranial vasculature (Figure 3C).
Diagnosis
Reversible cerebral vasoconstriction syndrome (RCVS)
Discussion
RCVS is a complex neurovascular disorder that has been increasingly recognized as a unique clinical radiological syndrome in the past couple of decades. The disorder is characterized by diffuse and segmental cerebral artery vasoconstriction, often in medium-sized vessels located in the circle of Willis.1,2 As a result of the widely distributed vasoconstriction, several infarcts may be present in neuroimaging.2
The hallmark symptom of RCVS is thunderclap headaches. These are often short-lived, lasting one to three hours, with some as brief as only a few minutes and others lasting several days. Over 94% of patients will report thunderclap headaches as their primary symptom, with many reporting several such headaches over the course of a one- to four-week period.3,4 Many patients also report chronic headaches or migraines at baseline. Other reported symptoms include either transient or permanent focal neurological deficits, as well as focal or generalized seizures, although headaches may be the only reported symptom.3
In addition to the presenting symptoms, there are several factors that should clue a clinician to the possibility that RCVS is on the differential. Women are disproportionately affected, with one study showing that over 80% of patients were female.5 Although it can affect people at a wide range of ages, the peak incidence occurs around 42 years of age.4 There are also several precipitating factors that have been found to be associated with the incidence of RCVS, including use of vasoactive drugs such as cannabis and cocaine, the postpartum period, recent sexual intercourse, as well as several medications including nasal decongestants, oral contraceptives, and antidepressants.2,5,6
CT and CT angiography are typically the first imaging studies done for patients presenting with thunderclap headaches, which allows clinicians to rule out other potential causes. The hallmark findings on angiography are the presence of multifocal stenoses as well as cerebral artery segments displaying alternating segments of severe vasoconstriction and dilation, often described as having a “string of beads” appearance.5,7 Other frequently seen complications on CT and MRI include multifocal ischemic lesions and cerebral hemorrhages, the most common of which are subarachnoid, as well as reversible brain edema hemorrhages.5,8
Although many patients have resolution of symptoms and complete recovery within three months of presentation, there is a risk of long-term complications. Amongst the most devastating of these complications are ischemic strokes, subarachnoid hemorrhages, posterior reversible encephalopathy syndrome, and seizures.5,9
Due to the risk of these complications, treatment of RCVS is paramount in improving patient outcomes. Although no randomized control trials for treatment options have been done, several cases have shown that the use of calcium-channel antagonists, most commonly nimodipine and verapamil, have been found to be safe and well-tolerated medications associated with resolution of thunderclap headaches.10,11
Mina Botros, BS, is a medical student at University of Massachusetts Chan Medical School in Worcester, Massachusetts.
Jasmeet Singh, MD, is a professor in the division of neurointerventional radiology, department of radiology at University of Massachusetts Medical Center in Worcester, Massachusetts.
Anna Luisa Kuhn, MD, PhD, is an associate professor in the division of neurointerventional radiology, department of radiology at University of Massachusetts Medical Center in Worcester, Massachusetts.
References
1. Chen SP, Wang SJ. Pathophysiology of reversible cerebral vasoconstriction syndrome. J Biomed Sci. 2022;29(1):72.
2. Ribas MZ, Paticcié GF, de Medeiros SDP, de Oliveira Veras A, Noleto FM, Dos Santos JCC. Reversible cerebral vasoconstriction syndrome: literature review. Egypt J Neurol Psychiatr Neurosurg. 2023;59(1):5.
3. Chen SP, Fuh JL, Wang SJ. Reversible cerebral vasoconstriction syndrome: an under-recognized clinical emergency. Ther Adv Neurol Disord. 2010;3(3):161-171.
4. Ducros A. Reversible cerebral vasoconstriction syndrome. Lancet Neurol. 2012;11(10):906-917.
5. Song TJ, Lee KH, Li H, et al. Reversible cerebral vasoconstriction syndrome: a comprehensive systematic review. Eur Rev Med Pharmacol Sci. 2021;25(9):3519-3529.
6. Ducros A, Boukobza M, Porcher R, Sarov M, Valade D, Bousser MG. The clinical and radiological spectrum of reversible cerebral vasoconstriction syndrome. A prospective series of 67 patients. Brain. 2007;130(pt 12):3091-3101.
7. Bernard KRL, Rivera M. Reversible cerebral vasoconstriction syndrome. J Emerg Med. 2015;49(1):26-31.
8. Pilato F, Distefano M, Calandrelli R. Posterior reversible encephalopathy syndrome and reversible cerebral vasoconstriction syndrome: clinical and radiological considerations. Front Neurol. 2020;11:34.
9. Calabrese LH, Dodick DW, Schwedt TJ, Singhal AB. Narrative review: reversible cerebral vasoconstriction syndromes. Ann Intern Med. 2007;146(1):34-44.
10. Cappelen-Smith C, Calic Z, Cordato D. Reversible cerebral vasoconstriction syndrome: recognition and treatment. Curr Treat Options Neurol. 2017;19(6):21.
11. Collins L, Lam L, Kleinig O, et al. Verapamil in the treatment of reversible cerebral vasoconstriction syndrome: a systematic review. J Clin Neurosci. 2023;113:130-141.
