By Pallav Shah, MD, and Lyle R. Gesner, MD
History
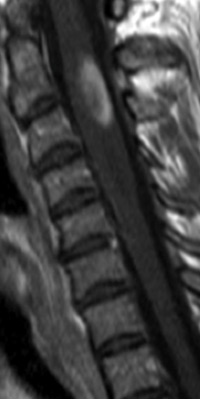
A 47-year-old female presents with hilar adenopathy, perilymphatic reticulonodular infiltrates and upper-extremity weakness.
Diagnosis
Intramedullary sarcoid
Clinical
• Idiopathic systemic disease is characterized by noncaseating granulomas and proliferation of epitheliod cells; young and middle-aged women are disproportionately affected.
• Neurologic symptoms occur in 5% of affected individuals. Autopsy reports indicate neurologic involvement in up to 27% of cases, perhaps a reflection of subclinical disease.
• Intramedullary sarcoid most commonly presents with weakness; distribution of symptoms is dependent upon cord level affected. Nearly 50% of patients have simultaneous intracranial involvement.
Findings
• T2WI demonstrates expansile, hyperintense intramedullary signal between C2-C5; T1WI postcontrast image demonstrates ovoid enhancing region at C2-C3 (Figures 1 and 2).
• After 500 mg of IV methylprednisolone and a repeat MRI one week after admission, STIR sequence demonstrates substantial resolution of intramedullary signal change and cord swelling; enhancement also diminished in extent (Figures 3 and 4).
Key Diagnostic Features
• T2WI and STIR sequences demonstrate expansile, intramedullary hyperintense signal abnormality.
• Postcontrast T1WI typically reveals nodular focus of enhancement that corresponds to the focal sarcoid granuloma with surrounding lymphocytic infiltrates.
Differential Diagnosis
Demyelination, neoplasm, vacuolar myelopathy, intramedullary tuberculosis, or fungal infection
Treatment
Systemic corticosteroids, cyclophosphamide (Cytoxan); it is important to remember that resolution of MR findings lags behind clinical improvement.
— Pallav Shah, MD, is a diagnostic radiology resident at Saint Barnabas Medical Center in Livingston, New Jersey.
— Lyle R. Gesner, MD, is section chief of neuroradiology and radiology residency program director at Saint Barnabas Medical Center.
Suggested Reading
Christoforidis GA, Spickler EM, Recio MV, Mehta BM. MR of CNS sarcoidosis: correlation of imaging features to clinical symtpoms and Response to treatment. AJNR. 1999;20(4):655-669.
Koyama T, Ueda H, Togashi K, et al. Radiologic manifestations of sarcoidosis in various organs. Radiographics. 2004;24(1):87-104.
 |
 |
| Figure 1 | Figure 2 |
 |
 |
| Figure 3 | Figure 4 |
Submission Instructions
Submit cases directly to Rahul V. Pawar, MD, DABR (section editor for “On the Case”) at rvp325@yahoo.com. Cases submitted should be relevant and interesting. All modalities and subspecialties within radiology are equally considered.
Case submission entails two PowerPoint slides:
SLIDE 1
a. History (one-line phrase)
b. Two to five high-quality images in JPEG format without annotations
c. Name(s) of the author(s) (three maximum) and respective institutions
SLIDE 2
a. Diagnosis
b. Concise bulleted discussion (one to two lines each), including the following: pertinent clinical history, diagnostic imaging findings, differential diagnoses, treatment (if applicable)
c. Two to three relevant and current references, preferably citing peer-reviewed radiology literature
Department of Radiology, Division of Neuroradiology
Saint Barnabas Medical Center/Barnabas Ambulatory Care Center