‘Not Just a Diagnosis in Children’
History
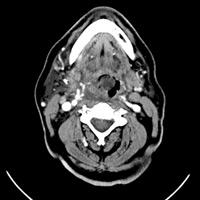
A 68-year-old man presented to the emergency department (ED) with one day of rapidly progressive throat pain. The patient reported rhinorrhea within the preceding few days, which was followed by mild difficulty swallowing and sore throat. Upon reporting to his primary care physician, the patient was febrile to 102 and instructed to visit the ED, where physical examination revealed exquisite tenderness along the anterior and right ventrolateral neck at the level of the mandible. A CT scan of the neck with contrast was performed.
Although vital signs were initially stable, the patient’s blood pressure began to drop precipitously into the 70s/30s. IV access was secured; pressors and IV fluids with antibiotics were initiated, and the patient was transferred to the ICU. The otolaryngology service opted against emergent intubation and followed with close observation.
Findings
Multiplanar images from a CT scan of the neck with IV contrast demonstrated asymmetric narrowing of the airway secondary to mucosal thickening and submucosal edema involving the oropharynx, hypopharynx, and supraglottic larynx (Figures 1A, B, and C). The right vallecula and pyriform sinus were nearly obliterated. Perhaps the most striking finding was a masslike swelling/inflammation of the epiglottis and contiguous aryepiglottic fold. There was also infiltration of pre-epiglottic fat. No tonsillar or retropharyngeal suppurative adenitis or abscess was identified. Scattered nodes within the adjacent cervical stations were appreciated, none of which met pathologic size criteria.
Diagnosis
Acute epiglottitis (AE)
Discussion
Epiglottitis in children is a well-known entity that has potentially life-threatening implications (ie, rapid airway compromise). A high degree of suspicion is warranted in the pediatric setting, so emergent intubation and antibiotics are initiated promptly.
With the advent of a vaccination against Haemophilus influenza type b (Hib), the incidence of childhood AE has diminished substantially. Some epidemiological studies, however, have demonstrated worrisome trends regarding a resurgence of AE in older children and nonimmunized cohorts.1
The incidence of AE in adults is uncommon and therefore often unrecognized, even in the emergent setting. Although the clinical course is typically milder compared with children, prompt therapy and surveillance are required. Most adults have no signs of airway obstruction, yet the clinical threshold for airway management should be low, since it may remain the only means to prevent death in dire circumstances.2
Adults often present with fever, stridor, and sore throat. More ominous symptoms include odynophagia, shortness of breath, and drooling. Clinical examination should include radiographs of the neck/upper airway and direct fiberoptic laryngoscopy.3 It has been postulated that airway collapse occurs less frequently in adults because of the anatomic configuration (ie, larger diameter and more rigid structures of the adult airway).4
Nemzek et al attempted to define the radiologic parameters of AE on plain radiography using internal reference standards. They deemed the ratio of the width of the epiglottis relative to the anteroposterior width of C4 should not exceed 0.33, with sensitivity and specificity values equaling 96% and 100%, respectively.5
CT scanning of the neck is useful to delineate the extent of airway involvement as well as to exclude the presence of additional and/or other processes. Inflammation and swelling of the oropharynx is common with AE in adults, termed supraglottitis, and encompasses the base of the tongue, soft palate, uvula, and valleculae. Enlargement of the epiglottis, aryepiglottic folds, and arytenoids can be visually more dramatic and conclusive than plain films. Identification of suppurative adenitis and/or abscess is often the main indication for CT of the neck with contrast. Under these conditions, IV antibiotics alone will not suffice, with surgical drainage becoming the mainstay of treatment. In patients where direct laryngoscopy cannot be performed, CT also remains an easy alternative.6
Empiric antibiotics, IV hydration, and close observation of airway stability are fundamental to management of AE in adults. Only a minority of patients require intubation. Outcomes are generally favorable if clinicians and radiologists operate in concert to establish a diagnosis and initiate the appropriate therapy.
— Rahul V. Pawar, MD, DABR, is an attending neuroradiologist at Saint Barnabas Medical Center in Livingston, N.J.
 |
 |
| Figure 1 A—Axial image | Figure 1B—Sagittal image |
 |
|
| Figure 1C—Coronal image |
REFERENCES
- McVernon J, Trotter CL, Slack MP, Ramsay ME. Trends in Haemophilus influenza type b infections in adults in England and Wales: Surveillance study. BMJ. 2004;329(7467):655-658.
- Wick F, Ballmer PE, Haller A. Acute epiglottitis in adults. Swiss Med Wkly. 2002;132(37-38):541-547.
- Sack JL, Brock CD. Identifying acute epiglottitis in adults. High degree of awareness, close monitoring are key. Postgrad Med. 2002;112(1):81-82, 85-86.
- Hawkins DB, Miller AH, Sachs GB, Benz RT. Acute epiglottitis in adults. Laryngoscope. 1973;83(8):1211-1220.
- Nemzeck WR, Katzberg RW, Van Slyke MA, et al. A reappraisal of the radiologic findings of acute inflammation of the epiglottis and supraglottic structures in adults. AJNR. 1995;16(3):495-502.
- Smith MM, Mukherji SK, Thompson JE, Castillo M. CT in adult supraglottitis. AJNR. 1996;17(7):1355-1358
ON THE CASE submission requirements
- Cases should have clinical relevance and clear radiological findings.
- Sections should include a title, history and course of illness, findings, diagnosis, and discussion.
- Maximum word limit should not exceed 800. At least three references are recommended.
- Cases may be submitted from any radiological subspecialty and imaging modality.
- Figures must be high-quality JPEG or TIFF images and labeled for ease of reference. Please keep images in their native format, without the addition of arrows or other means of highlighting the key findings.