By Rahul V. Pawar, MD
History
A 59-year-old woman was referred to an otolaryngologist, a specialist of the ear, nose, and throat (ENT), for right-sided facial pain. In brief, her primary complaint was periodic, intense pain/discomfort along the right side of her face, generalizing to the orbital region and malar eminence. She specifically characterized the pain as having a “stabbing” or “piercing” quality. A review of symptoms and physical exam more or less excluded other disorders, including tension headache, classic migraine, temporomandibular joint dysfunction, etc.
Findings
The initial noncontrast CT head was negative. The ENT surgeon ordered a dedicated MRI of the brain and internal auditory canal with and without IV contrast. Pertinent negatives included no space-occupying lesions, white matter lesions, infarct, hemorrhage, hydrocephalus, or extra-axial collection.
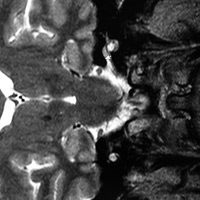
Careful review of the thin-slice, T2 weighted axial/coronal images through the brainstem/posterior fossa did reveal contact between the right trigeminal nerve root entry zone (REZ) and a tiny, serpentine vessel coursing in very close proximity.
Diagnosis
Trigeminal neuralgia (TN) presumably secondary to neurovascular contact (ie, nerve-vessel conflict).
Discussion
Trigeminal neuralgia, also known as tic douloureux, has been exhaustively discussed in the literature. Dating back to research from 1989, Tash, et al. concluded that MR imaging imaging should play a role in the workup of patients with TN since neurovascular contact may be present even if asymptomatic in some patients. Neurovascular compression is the main cause of TN. Facial pain can involve V1, V2, and/or V3 divisions of the trigeminal nerve. In the majority of cases, compression is caused by a tortuous superior cerebellar artery. Other branches of the vertebrobasilar circulation may be implicated, as well.
Etiologies for TN referable to the brain stem may include multiple sclerosis, infarct, or neoplasm. Cisternal etiologies include nerve-vessel conflict (aforementioned), but extrinsic compression from space-occupying lesions (eg, schwannomas, meningiomas, epidermoids, metastases) can present similarly. Pathology within the Meckel cave and/or cavernous sinus bears a similar differential akin to lesions that can affect the cisternal segment with the inclusion of pituitary masses and internal carotid artery aneurysms. Perineural spread of disease along trigeminal nerve branches from head/neck malignancies can also incite TN.
Very uncommon, if not rare, etiologies may induce compression and/or irritation of the trigeminal REZ. In Case Reports in Anesthesiology, Bang et al recently published a case of TN induced by ossification of the tentorium cerebelli overlying the trigeminal notch.
Common neurosurgical treatments for TN include microvascular decompression (MVD) and gamma-knife radiosurgery. In a study published in the Journal of Clinical Neuroscience designed to evaluate the long-term efficacy of MVD and radiosurgery with respect to pain relief and patient satisfaction, MVD offered total pain relief in a significantly higher number of patients compared with radiosurgery.
— Rahul V. Pawar, MD, Department of Radiology, Division of Neuroradiology, is Clinical Assistant Professor, UMDNJ—New Jersey Medical School.
 |
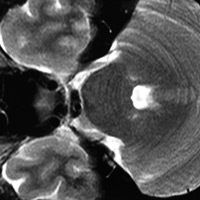 |
| Figure 1 | Figure 2 |
References
- Tash RR, Sze G, Leslie DR. Trigeminal neuralgia: MR imaging features. Radiology. 1989;172(3):767-770.
- Majoie CB, Verbeeten B Jr, Dol JA, Peeters FL. Trigeminal neuropathy: evaluation with MR imaging. Radiographics. 1995;15(4):795-811.
- Bang SW, Han KR, Kim SH, et al. Uncommon cause of trigeminal neuralgia: tentorial ossification over trigeminal notch. Case Rep Anesthesiol. 2015;2015:819354.
- Nanda A, Javalkar V, Zhang S, Ahmed O. Long term efficacy and patient satisfaction of microvascular decompression and gamma knife radiosurgery for trigeminal neuralgia. J Clin Neurosci. 2015;22(5):818-822.
Submission Instructions
- Cases should have clinical relevance and clear radiological findings.
- Seconds should include a title, history and course of illness, findings, diagnosis, and discussion.
- Word count should not exceed 800. At least three references are recommended.
- Cases may be submitted from any radiological subspecialty and imaging modality.
- Figures must be high-quality JPEG or TIFF images and labeled for ease of reference. Please keep images in their native format, without the addition of arrows or other means of highlighting the key findings.
Submit cases via e-mail to Rahul V. Pawar, MD, at rvp325@gmail.com or to Radiology Today at jknaub@gvpub.com.
Department of Radiology, Division of Neuroradiology
Saint Barnabas Medical Center/Barnabas Ambulatory Care Center