By Rahul V. Pawar, MD, and Kimmerle A. Pawar, MD, MPH
History
37-year-old woman with a body mass index (BMI) of 31 and no other pertinent medical history presented to the emergency department with severe, throbbing headaches. Detailed history of present illness revealed occasional eye pain, usually on the left side. Subjectively, no change in vision was appreciated. The patient denied any neurologic history (eg, no prior ischemic insult, seizure). Following a review of systems and physical exam, the patient was deemed neurologically intact. She was afebrile and no meningeal signs were present. Ophthalmology was consulted because of the asymmetric eye pain/discomfort that accompanied her periodic headaches. CT and MRI were ordered.
Findings
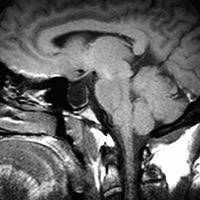
Initial nonenhanced CT screening was negative, with no obvious findings reported prospectively. Follow-up MRI seemed negative at first glance, as well. No intracranial mass, vascular lesion, hydrocephalus, or extra-axial collection was evident. However, midline sagittal T1 weighted MRI (Figure 1) revealed an expanded, largely fluid-filled sella turcica with a thin mantle of pituitary tissue—a partially empty sella. Axial T2 weighted MRI (Figure 2) through the orbits demonstrated striking posterior globe/scleral flattening, prominence of the perioptic cerebrospinal fluid (CSF) and optic nerve sheath tortuosity.
Diagnosis
Pseudotumor cerebri (PTC)/idiopathic intracranial hypertension
Discussion
PTC most often manifests with headaches and sometimes with vision changes. Demographically, women of childbearing age are affected most commonly; the female to male ratio is 8:1 in the literature. Obesity is a strong risk factor as well. Some have concluded that the odds ratio of PTC increases substantially in patients with a BMI of 35 or greater compared with patients with a BMI between 25 and 29. Weight loss, including procedures such as gastric bypass to augment weight reduction, can dramatically reduce the risk and recurrence of PTC.1
Mechanistically, dural sinus stenosis and PTC are believed to have a strong correlation. Whether venous stenosis is the cause or result of PTC has been debated. In any case, venous sinus stenting has proven to be an efficacious treatment for PTC, especially in the acute setting. In 2015, Elder and colleagues reported that urgent transverse venous stenting in the acute setting may be critical to preserve vision.2 Three out of four patients that presented with acute vision loss secondary to PTC demonstrated improvement in visual parameters following stenting.
Therapeutic lumbar puncture can relieve symptoms temporarily and serve as a bridge to stenting and/or longer term management such as weight loss. Sonographic measurement of optic nerve sheath diameter (ONSD) has been shown to be a reliable, noninvasive method to characterize elevated intracranial pressure (ICP) in a variety of settings. Singleton and colleagues showed that sonographic measurement of ONSD reduction may be a novel, noninvasive, and convenient way to follow acute reductions in ICP.3 ONSD measurements correlated with ICP as measured by opening and closing lumbar puncture pressures and showed an acute reduction in ONSD within 30 minutes after lumbar puncture. Note that “documented elevated ICP were measured in the lateral decubitus position; in addition, findings of assessment of ICP by lumbar puncture should be considered abnormal if they are above 20 cm H2O in normal-weight individuals and 25 mm H2O in obese individuals.”1
Imaging plays a pivotal role in the diagnosis of PTC. The ACR recommends MRI of the brain and orbits in patients that present with any vision dysfunction. Conventional MR findings that may reflect PTC include posterior globe flattening, enlarged perioptic CSF space, optic nerve tortuosity, empty sella/partially empty sella, intraocular protrusion of the optic nerve head, and slitlike ventricles. Transverse sinus stenosis may be seen upon MR venography. Findings that have the highest sensitivities and specificities include posterior globe/scleral flattening, enlarged perioptic CSF space, partially empty sella (seen with long-standing PTC) and optic nerve tortuosity.
— Kimmerle A. Pawar, MD, MPH, is a board-certified, attending emergency medicine physician at Saint Barnabas Medical Center, Livingston, New Jersey.
 |
 |
| Figure 1 | Figure 2 |
References
- Degnan AJ, Levy LM. Pseudotumor cerebri: brief review of clinical syndrome and imaging findings. AJNR Am J Neuroradiol. 2011;32(11):1986-1993.
- Elder BD, Rory Goodwin C, Kosztowski TA, et al. Venous sinus stenting is a valuable treatment for fulminant idiopathic intracranial hypertension. J Clin Neurosci. 2015;22(4):685-689.
- Singleton J, Dagan A, Edlow JA, Hoffmann B. Real-time optic nerve sheath diameter reduction measured with bedside ultrasound after therapeutic lumbar puncture in a patient with idiopathic intracranial hypertension. Am J Emerg Med. 2015;33(6):860.e5-860.e7.
Submission Instructions
- Cases should have clinical relevance and clear radiological findings.
- Seconds should include a title, history and course of illness, findings, diagnosis, and discussion.
- Word count should not exceed 800. At least three references are recommended.
- Cases may be submitted from any radiological subspecialty and imaging modality.
- Figures must be high-quality JPEG or TIFF images and labeled for ease of reference. Please keep images in their native format, without the addition of arrows or other means of highlighting the key findings.
Submit cases via e-mail to Rahul V. Pawar, MD, at rvp325@gmail.com or to Radiology Today at jknaub@gvpub.com.
Department of Radiology, Division of Neuroradiology
Saint Barnabas Medical Center/Barnabas Ambulatory Care Center