By Anna Luisa Kühn, MD, PhD
History
A 75-year-old male without significant past medical history presented with acute chest pain to the emergency department and was diagnosed with non-ST segment elevation myocardial infarction. The patient was admitted to the hospital and placed on a heparin drip in anticipation of cardiac catheterization. Three days after the admission, the patient complained of new onset testicular pain and progressive testicular swelling.
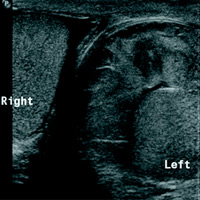
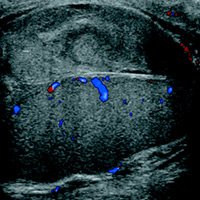
Findings
Sonographic comparison view of both testicles and sagittal grayscale ultrasound of the left testicle demonstrate a complex heterogeneous collection around the left testicle. There is associated mass effect on the left testicle, but color Doppler evaluation shows preserved intratesticular blood flow. The testicular parenchyma is normal.
Diagnosis
Acute extratesticular hematoma/hematocele.
Discussion
An extratesticular hematocele is a collection of blood in the scrotal sac, specifically in the tunica vaginalis but outside of the testicle. Sonographic appearance of a hematocele varies with age of the collection, from echogenic in the acute phase to a more hypoechogenic pattern with possible cystic degeneration, debris, and septations in the subacute to chronic phase.1
Iatrogenic causes of extratesticular hematoceles, aside from complication with anticoagulation therapy, include postoperative complications after inguinal hernia repair or orchiectomy.2,3
Acute onset of a large hematocele can mimic testicular torsion due to the mass effect on the testicle and compromise of blood flow.4 Evacuation of the hematoma is indicated for symptom relief and restoration of normal intratesticular blood flow.
Differential Diagnosis
Medical/surgical history and clinical presentation usually suggest the diagnosis, especially in the acute phase. Additionally, sonographic features of an acute hematoma are most often characteristic.
In other cases, particularly in those with atypical presentation, consideration of differential diagnoses including multicystic testicular tumors such as cystadenoma/cystadenocarcinoma of the rete testis and complicated testicular abscess are warranted.
— Anna Luisa Kühn, MD, PhD, is a second-year radiology resident at the University of Massachusetts Medical School in Worcester, Massachusetts.
 |
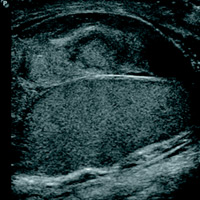 |
| Figure 1 | Figure 2 |
 |
|
| Figure 3 |
References
- Bhatt S, Dogra VS. Role of US in testicular and scrotal trauma. Radiographics. 2008;28(6):1617-1629.
- Deurdulian C, Mittelstaedt CA, Chong WK, Fielding JR. US of acute scrotal trauma: optimal technique, imaging findings, and management. Radiographics. 2007;27(2):357-369.
- Archer A, Choyke PL, O’Brien W, Maxted WC, Grant EG. Scrotal enlargement following inguinal herniorrhaphy: ultrasound evaluation. Urol Radiol. 1988;9(4):249-252.
- Dogra VS, Bhatt S, Rubens DJ. Sonographic evaluation of testicular torsion. Ultrasound Clin. 2006;1(1):55-66.
Submission Instructions
- Cases should have clinical relevance and clear radiological findings.
- Seconds should include a title, history and course of illness, findings, diagnosis, and discussion.
- Word count should not exceed 800. At least three references are recommended.
- Cases may be submitted from any radiological subspecialty and imaging modality.
- Figures must be high-quality JPEG or TIFF images and labeled for ease of reference. Please keep images in their native format, without the addition of arrows or other means of highlighting the key findings.
Submit cases via e-mail to Rahul V. Pawar, MD, at rvp325@gmail.com or to Radiology Today at jknaub@gvpub.com.
Department of Radiology, Division of Neuroradiology
Saint Barnabas Medical Center/Barnabas Ambulatory Care Center