Multiple Cerebral Abscesses in a Patient with Diabetes Mellitus and Endocarditis
HISTORY AND COURSE OF ILLNESS
A 74-year-old diabetic male was transferred to our institution with a diagnosis of embolic cerebral abscesses presumably secondary to endocarditis. A non-contrast CT scan performed at the outside hospital demonstrated multiple foci of abnormal attenuation concerning for metastatic disease or abscesses. Neurological examination was positive for moderate motoric deficits. Physical examination demonstrated a systolic murmur and a solitary splinter hemorrhage beneath a nail bed involving his right hand. A transesophageal echocardiogram demonstrated an echogenic mobile mass affixed to the atrial margin of the mitral valve, consistent with a vegetation. Empiric intravenous antibiotics were initiated after blood cultures were drawn. Upon arrival at our institution, a contrast-enhanced CT scan of the chest, abdomen and pelvis excluded primary underlying neoplasm. Subsequent MRI of the brain was performed to further characterize the multifocal lesions initially discovered by CT.
FINDINGS
Post-contrast T1WI reveals multiple nodular and ring-enhancing lesions centered at the corticomedullary junction with accompanying deep white matter involvement (i.e. genu of the corpus callosum) (Figure 1). T2WI demonstrates hyperintense lesions with a relatively hypointense rim (Figure 2). Majority of the lesions also demonstrate hyperintense signal on the trace diffusion images with corresponding ADC deficit (Figure 3).
DIAGNOSIS
Pyogenic cerebral abscesses secondary to bacterial endocarditis.
Blood cultures were positive for ceftriaxone-sensitive Acinetobacter. MRI suggested the presence of multiple cerebral abscesses. Although a pathologic diagnosis was not obtained, the size and number of the nodular/ring-enhancing lesions were documented by serial MRI examinations. With continuous intravenous antibiotic treatment, the lesions progressively diminished in size and enhancement. Serial echocardiograms also confirmed resolution of the mitral valve vegetation. Ultimately, the patient improved and was enrolled in a rehabilitation program with only mild persistent neurologic deficits.
DISCUSSION
Ring-enhancing lesions in the brain yield a broad differential diagnosis. Metastatic disease, abscess, multifocal glioma, subacute infarction, contusion, tumefactive demyelination, resolving hematoma and radiation necrosis can have overlapping imaging characteristics. In clinical practice, history is often suggestive and imaging serves to either confirm or negate the presence of intracranial disease. Differentiation between infection and metastatic disease is critical, since untreated cerebral abscesses can rapidly be fatal. Sources of embolic disease are most commonly indwelling catheters, foreign devices and acute/subacute endocarditis.
Although imaging can be non-specific, there are certain characteristics that may be helpful in limiting the differential. Abscesses from embolic disease are typically distributed at the gray-white matter junction within the vascular territory of the middle cerebral arteries. Post-contrast T1WI and T2/FLAIR sequences reveals the presence of multiple nodular/ring-enhancing and hyperintense lesions, respectively (often < 2 cm)1 (See Figures 1 and4). Once mature, abscesses demonstrate a well-defined capsule that is T2 hypointense.2 Diffusion weighted imaging routinely serves to differentiate between abscesses and metastatic disease. Usually, abscesses will reveal evidence of abnormal restricted diffusion (hyperintense signal on the trace images, with corresponding ADC deficit). It has been postulated that viscous pus within the abscess cavity serves to limit the extracellular movement (mean diffusivity) of water molecules. Albeit widely considered to be pathognomonic for abscess, low ADC values are not 100% specific for brain abscess since occasionally, restricted water diffusion might be found in metastatic deposits.3 More advanced imaging techniques can be adopted if the diagnosis remains in question. Perfusion MR, which calculates the cerebral blood volume (rCBV) relative to contralateral normal-appearing white matter, can differentiate between abscess and neoplasm with high certainty. The mean rCBV of peripheral tumor wall is significantly larger compared with mean values obtained from pyogenic abscess wall.4
— Rahul V. Pawar, MD is a board-certified diagnostic radiologist completing a fellowship in Neuroradiology at New York University Langone Medical Center. Kimmerle A. Pawar MD, MPH is completing her residency in Emergency Medicine at Bellevue Hospital Center, NYU Langone Medical Center.
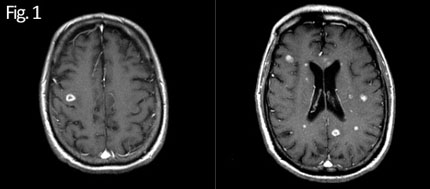
Post-contrast T1WI — Multiple nodular and ring-enhancing lesions at corticomedullary junction and deep white matter
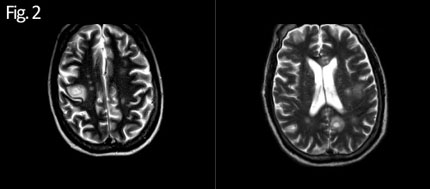
T2WI— Multiple hyperintense lesions at corticomedullary junction Well-defined hypointense rim (abscess wall)
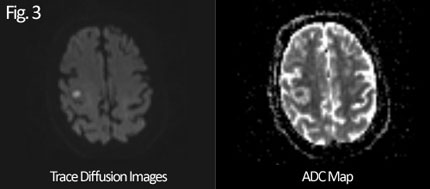
Lesions are hyperintense on trace images (with corresponding ADC deficit (low signal). Compatible w/ “abnormal restricted diffusion”
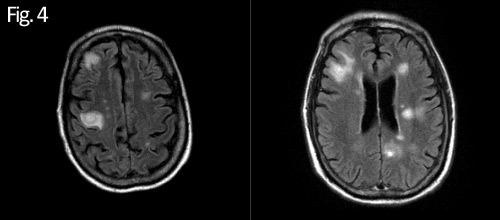
FLAIR sequence — Multiple nodular hyperintense lesions at corticomedullary junction & deep white matter
REFERENCES
- Smirniotopoulos JG, Contrast Enhancement in the Brain and Meninges. Radiographics 2007; 27:525-551.
- Fertikh D, Krejza J, Cunqueiro A, et al. Discrimination of capsular stage brain abscesses from necrotic or cystic neoplasms using diffusing-weighted magnetic resonance imaging. J Neurosurg 2007 January; 106: 76-81.
- Hartmann,M, Jansen O, Heiland S, et al. Restricted Diffusion within Ring Enhancement is Not Pathognomonic for Brain Abscess. AJNR 2001 October; 22: 1738-1742.
- Chan JH, Tsui EY, Chau LF, et al. Discrimination of an infected brain tumor from a cerebral abscess by combined MR perfusion and diffusion imaging. Comput Med Imaging Graph 2002 Jan-Feb; 26 (1): 19-23.
ON THE CASE submission requirements
- Cases should have clinical relevance and clear radiological findings.
- Sections should include a title, history and course of illness, findings, diagnosis, and discussion.
- Maximum word limit should not exceed 800. At least three references are recommended.
- Cases may be submitted from any radiological subspecialty and imaging modality.
- Figures must be high-quality JPEG or TIFF images and labeled for ease of reference. Please keep images in their native format, without the addition of arrows or other means of highlighting the key findings.