By Rahul V. Pawar, MD
History
A 10-year-old boy underwent neuroimaging after suffering a single (witnessed) seizure while at school; a brief episode of “staring” was followed by generalized convulsions.
Past medical history was significant for pervasive developmental disorder with autistic features. The patient was born prematurely (36 weeks) secondary to fetal distress.
On exam, he was alert but nonverbal, demonstrated poor eye contact, and was unable to obey commands. Mood and affect also were abnormal.
Findings
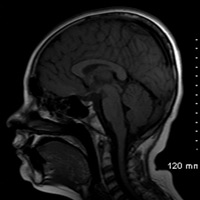
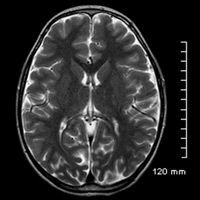
Compared with an age-matched, normal-appearing corpus callosum (Figure B), midline sagittal T1-weighted imaging of this patient’s brain demonstrated diminutive caliber of the posterior thirds corpus callosal body and splenium (Figure A). On careful inspection, a clearly definable callosal rostrum was absent. Axial T2-weighted imaging (Figure C) and coronal T1-weighted imaging (Figure D) both confirmed thinning of the posterior callosal body and splenium, secondary enlargement of the superior vermian cistern, and relatively parallel orientation of the lateral ventricles.
Diagnosis
Partial agenesis of the corpus callosum
Discussion
Formation of the corpus callosum—the largest commissural white matter structure in the brain—is complex. Rakic and Yavovlev concluded that “development of the corpus callosum is preceded by the infolding of the dorsal part of the lamina reuniens of His (1904) in the region of the prospective hippocampus into a median groove, and by fusion of its banks into a massa commissuralis which becomes the bed for corpus callosum.”1
Agenesis of the corpus callosum has been defined as the most common cerebral malformation.2 It is generally accepted that the corpus callosum forms anterior to posterior, beginning with the genu, followed by the body, splenium, and finally the rostrum.3 Interestingly, Kier and Truwit have postulated the converse, reporting that the corpus callosum actually develops bidirectionally.4
Pediatric neuroimaging plays a seminal role in a comprehensive semiologic workup. With particular respect to the corpus callosum, MRI has a distinct advantage over CT since the intrinsic T1 hyperintensity of callosal myelin enables identification of subtle abnormalities.5 Images depicted were generated on the Philips Intera 1.5T MRI system.
Clinically, the presentation of corpus callosum agenesis is variable; the spectrum includes those who may be (relatively) asymptomatic as well as patients who suffer from severe mental retardation. A constellation of associated behavioral and psychiatric disorders have been reported, including mood disturbances, attention-deficit/hyperactivity disorder, and autistic features. Epilepsy is a frequent manifestation that presents during early childhood and is generally controllable with antiepileptic medications.6
— Rahul V. Pawar, MD, is a diagnostic neuroradiologist at Saint Barnabas Medical Center in Livingston, New Jersey, and a consultant for Philips Healthcare North America.
 |
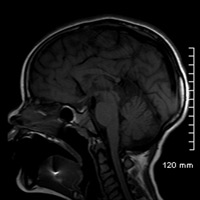 |
| Figure A | Figure B |
 |
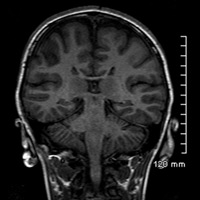 |
| Figure C | Figure D |
- Rakic P, Yakovlev PI. Development of the corpus callosum and cavum septi in man. J Comp Neurol. 1968;132(1):45-72.
- Jeret JS, Serur D, Wisniewski KE, Lubin RA. Clinicopathological findings associated with agenesis of the corpus callosum. Brain Dev. 1987;9(3):255-264.
- Barkovich AJ, Norman D. Anomalies of the corpus callosum: correlation with further anomalies of the brain. AJR Am J Roentgenol. 1988;151(1):171-179.
- Kier EL, Truwit CL. The normal and abnormal genu of the corpus callosum: an evolutionary, embryologic, anatomic, and MR analysis. AJNR Am J Neuroradiol. 1996;17(9):1631-1641.
- Davidson HD, Abraham R, Steiner RE. Agenesis of the corpus callosum: magnetic resonance imaging. Radiology. 1985;155(2):371-373.
- Moutard ML. Isolated corpus callosum agenesis. Orphanet Encyclopedia. https://www.orpha.net/data/patho/Pro/en/IsolatedCorpusCallosumAgenesis-FRenPro447.pdf. September 2003.
Submission Instructions
- Cases should have clinical relevance and clear radiological findings.
- Seconds should include a title, history and course of illness, findings, diagnosis, and discussion.
- Word count should not exceed 800. At least three references are recommended.
- Cases may be submitted from any radiological subspecialty and imaging modality.
- Figures must be high-quality JPEG or TIFF images and labeled for ease of reference. Please keep images in their native format, without the addition of arrows or other means of highlighting the key findings.
Submit cases via e-mail to Rahul V. Pawar, MD, at rvp325@gmail.com or to Radiology Today at jknaub@gvpub.com.
Department of Radiology, Division of Neuroradiology
Saint Barnabas Medical Center/Barnabas Ambulatory Care Center